A breakthrough in HIV research, the role of CD28 in modulating T-cell functions uncovered
Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 16, 2024 7 months, 2 days, 11 hours, 27 minutes ago
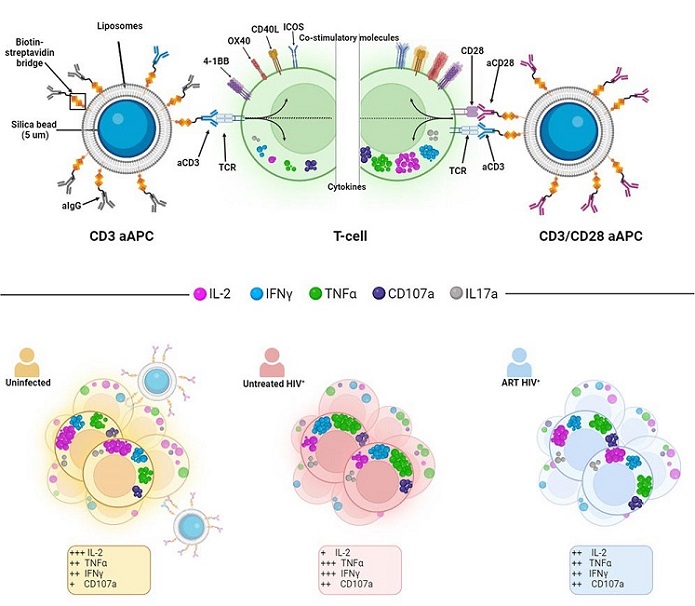
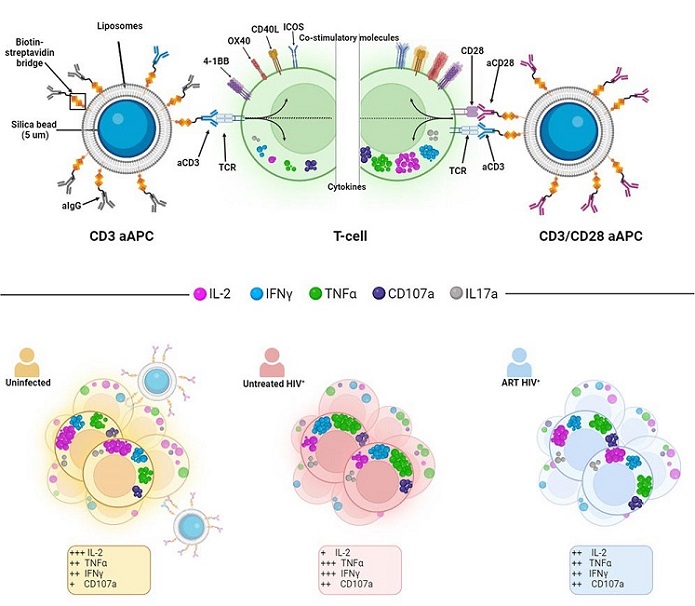
HIV News: Researchers from various renowned institutions have developed a novel Artificial Antigen-Presenting Cell (aAPC) system to explore how CD28, a key co-stimulatory molecule, influences T-cell functions during HIV infection. This groundbreaking study, conducted by experts from the Université de Montréal-Canada, McGill University Health Centre-Canada, and Lausanne University Hospital-Switzerland, reveals new insights into T-cell dysfunction and potential therapeutic approaches to improve immune responses in people living with HIV. This
HIV News report delves into the findings of the study, which showed how CD28 co-stimulation can modulate T-cell activity, offering potential strategies to enhance immune function during chronic HIV infection.
 Graphical Abstract. The role of CD28 in modulating T-cell functions during HIV infection uncovered
What are Artificial Antigen-Presenting Cells?
Graphical Abstract. The role of CD28 in modulating T-cell functions during HIV infection uncovered
What are Artificial Antigen-Presenting Cells?
Artificial Antigen-Presenting Cells (aAPCs) are laboratory-engineered systems designed to mimic the function of natural antigen-presenting cells. Natural APCs, such as dendritic cells, play a crucial role in immune responses by presenting foreign antigens to T cells, thereby activating them. However, natural APCs express a range of co-stimulatory molecules, making it difficult to study specific molecular interactions, such as those involving CD28.
To address this challenge, the researchers developed aAPCs composed of silica microbeads coated with lipid bilayers. These aAPCs were designed to mimic natural APCs by incorporating agonistic antibodies targeting CD3 and CD28, two molecules critical for T-cell activation. This system enabled the researchers to control the interactions between these molecules and study their effects on T-cell functions in isolation.
Study Findings: The Role of CD28 in T-cell Activation
The study aimed to investigate how CD28 co-stimulation affects the activation and function of CD4+ and CD8+ T cells in individuals with untreated (viremic) HIV infections. The researchers also examined how antiretroviral therapy (ART) influences these processes.
Key Findings:
-Cytokine Production: The aAPCs induced robust cytokine production in both CD4+ and CD8+ T cells. Upon stimulation, a significant upregulation of cytokines such as IL-2, IFNγ, TNFα, and CD107a was observed. Notably, IL-2 production was significantly enhanced by CD28 co-stimulation, highlighting its critical role in driving T-cell responses.
-Differences Between CD4+ and CD8+ T Cells: The study found distinct differences in how CD4+ and CD8+ T cells responded to CD28 co-stimulation. CD4+ T cells from HIV-infected individuals, both before and after ART, showed a skewed response toward producing TNFα and IFNγ, with diminished IL-2 production. In contrast, CD8+ T cells exhibited a more pronounced dependence on CD28 co-stimulation for IL-2 production.
-Impact of ART
strong>: While ART partially normalized the skewed cytokine profiles in CD4+ T cells, the same effect was not observed in CD8+ T cells. This suggests that CD8+ T cells may remain functionally impaired even after ART, contributing to the persistent immune dysfunction observed in many people living with HIV.
-Memory T Cells: CD28 co-stimulation played a particularly important role in the activation of memory T cells, especially those that had not been previously activated. This finding underscores the significance of CD28 in maintaining an effective immune memory response, which is crucial for long-term protection against infections.
Mechanisms Behind CD28's Role in T-cell Function
The study uncovered several key mechanisms by which CD28 co-stimulation modulates T-cell functions:
-Enhanced IL-2 Production: CD28 co-stimulation preferentially promoted the production of IL-2, a cytokine essential for T-cell proliferation and survival. This was achieved through enhanced transcription of the IL-2 gene and stabilization of its mRNA, ensuring sustained IL-2 production during T-cell activation.
-Modulation of Effector Functions: CD28 also fine-tuned the effector functions of T cells, promoting the production of cytokines such as IFNγ, TNFα, and CD40L. These cytokines play crucial roles in controlling viral infections and orchestrating immune responses.
-Selective Enrichment of T-cell Subpopulations: The study found that CD28 co-stimulation selectively enriched certain T-cell subpopulations, particularly those that produce IL-2. This suggests that CD28 helps shape the immune response by favoring the expansion of specific T-cell subsets with defined functions.
Implications for HIV Treatment
The findings from this study have significant implications for improving HIV treatment and management. Despite the effectiveness of ART in suppressing viral replication, many people living with HIV continue to experience immune dysfunction, particularly in their CD8+ T cells. This dysfunction may contribute to the higher risk of co-morbidities and reduced life expectancy in individuals with HIV.
By targeting CD28 co-stimulation, it may be possible to restore more balanced and functional T-cell responses in people with HIV. This approach could enhance the immune system's ability to control not only HIV but also other opportunistic infections and viruses that often complicate HIV infection, such as cytomegalovirus (CMV) and Epstein-Barr virus (EBV).
Future Directions: Customizing aAPC Systems
One of the most exciting aspects of this research is the potential to customize aAPC systems for a wide range of applications. In this study, the aAPCs were designed to stimulate T cells via CD3 and CD28, but other co-stimulatory molecules, such as CD40L and ICOS, could be incorporated to study their specific roles in T-cell activation.
Additionally, the aAPC system could be used to investigate T-cell dysfunction in other chronic viral infections, autoimmune diseases, and cancer. By identifying the key molecular pathways that regulate T-cell responses, researchers can develop targeted therapies to enhance immune function in a variety of disease contexts.
Conclusion
This study provides compelling evidence that CD28 co-stimulation plays a pivotal role in modulating T-cell functions during chronic HIV infection. The use of an artificial antigen-presenting cell system enabled the researchers to uncover critical insights into how CD28 influences cytokine production, effector functions, and T-cell memory responses.
While ART can partially restore immune function in people with HIV, the findings of this study suggest that additional interventions targeting CD28 co-stimulation may be necessary to fully restore immune balance, particularly in CD8+ T cells. These findings hold promise for improving HIV treatment and could pave the way for new therapies that enhance immune responses in people with HIV.
The study findings were published in the peer-reviewed journal: iScience.
https://www.sciencedirect.com/science/article/pii/S2589004224021722
For the latest HIV News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/sars-cov-2-reactivates-latent-hiv-and-can-influence-hiv-disease-progression
https://www.thailandmedical.news/news/new-insights-of-bone-health-in-hiv