Nikhil Prasad Fact checked by:Thailand Medical News Team Aug 19, 2024 1 year, 5 months, 3 weeks, 3 days, 7 hours, 3 minutes ago
Mpox News: As the world continues to battle various infectious diseases, monkeypox, a lesser-known but significant threat, has emerged, prompting scientists to investigate its origins, spread, and impact. Researchers from institutions including Biochem123 Education in London-UK, Rocket Biopharma Education-UK, and Imkers Brink in Germany have come together to shed light on the monkeypox virus (MPXV), tracing its roots and understanding its behavior.
 A deep dive into the immunopathogenesis of Mpox (Monkeypox) infections
A deep dive into the immunopathogenesis of Mpox (Monkeypox) infections
This
Mpox News delves into their findings, aiming to provide clear and understandable information on the monkeypox virus for everyone.
A Brief History of Monkeypox
Monkeypox was first identified in laboratory monkeys in Copenhagen in 1958, but it wasn't until 1970 that the first human case was reported in the Democratic Republic of the Congo (DRC). Initially confined to remote parts of Central and West Africa, the virus has now spread globally, raising concerns about its potential impact on public health. Monkeypox is caused by the monkeypox virus, a member of the Orthopoxvirus genus, which also includes the viruses responsible for smallpox and cowpox.
How Does Monkeypox Spread?
Monkeypox is a zoonotic disease, meaning it can be transmitted from animals to humans. The primary hosts of the virus include monkeys, squirrels, and rodents, but it can also spread from human to human through direct contact with infected bodily fluids, respiratory droplets, and contaminated materials. The virus enters the body through broken skin, the respiratory tract, or mucous membranes, such as the eyes, nose, or mouth. Recent studies are showing that some of the newer Mpox sub-lineages are better at airborne transmissions.
Unlike some other viruses, monkeypox does not have a specific receptor for cell entry. Instead, it uses various host proteins and receptors to facilitate its entry and replication within the body. Once inside, the virus hijacks the host's cellular machinery to produce more viral particles, leading to the symptoms associated with the disease.
Symptoms and Diagnosis of Monkeypox
Monkeypox typically presents with flu-like symptoms, including fever, headache, muscle aches, and exhaustion, followed by a rash that progresses from macules to papules, vesicles, pustules, and finally scabs. The rash often starts on the face before spreading to other parts of the body. Lymphadenopathy, or swollen lymph nodes, is another characteristic symptom that helps distinguish monkeypox from other similar diseases like chickenpox or smallpox.
Diagnosing monkeypox can be challenging, as its symptoms overlap with those of other diseases. Real-time polymerase chain reaction (PCR) tests, which detect the virus's genetic material, are the most reliable diagnostic tools currently available. These tests can confirm the presence of the monkeypox virus in various samples, including blood, saliva, and skin lesions.
;
The Global Spread of Monkeypox
Since the first human case was identified, monkeypox has remained largely confined to Africa. However, recent outbreaks in non-endemic countries, including the United States, the United Kingdom, and several European nations, have raised alarms. The World Health Organization (WHO) declared monkeypox a public health emergency in July 2022, underscoring the need for global vigilance.
Monkeypox is less contagious than diseases like COVID-19, with a basic reproduction number (R0) of around 1.39. This means that, on average, one infected person will transmit the virus to about 1.39 other people. For comparison, the R0 of measles is between 12 and 18, making it one of the most contagious diseases known.
Despite its lower transmission rate, monkeypox can still pose a significant risk, especially in vulnerable populations such as children, the elderly, and immunocompromised individuals. The fatality rate varies by viral clade, with the Congo Basin clade (clade I) being more virulent, having a fatality rate of up to 10%, while the West African clade (clade II) has a fatality rate of about 1% to 3.7%.
The Role of Immunology in Fighting Monkeypox
Immunology plays a crucial role in understanding and combating monkeypox, especially as the virus continues to spread to new regions and populations. The human immune system, a complex network of cells and molecules, is the body’s primary defense against pathogens like the monkeypox virus (MPXV). By studying how the immune system responds to MPXV, researchers can develop more effective vaccines and treatments, helping to curb the spread of the virus and reduce its impact on public health.
The Innate Immune Response: The First Line of Defense
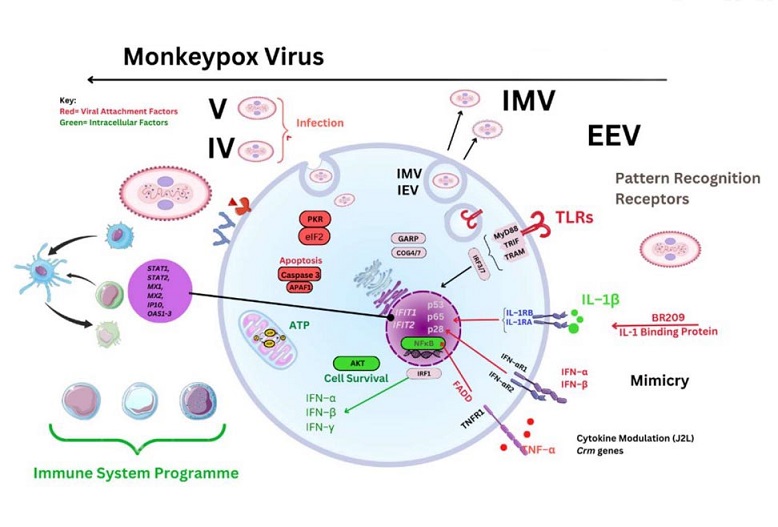
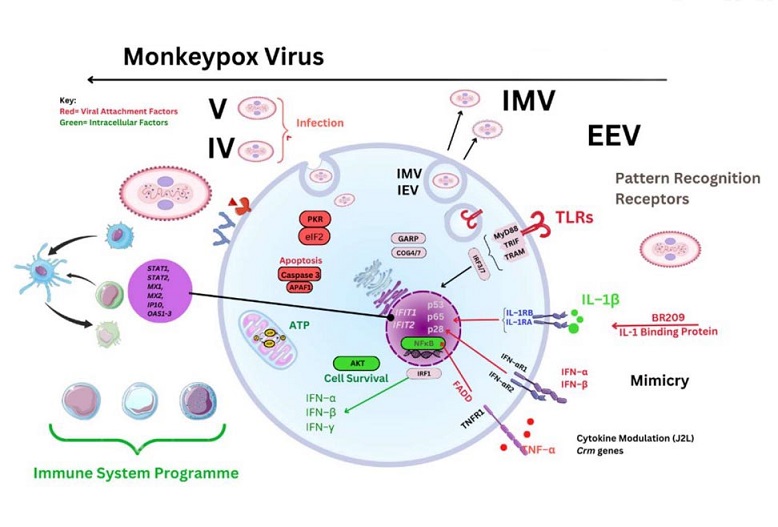
The immune response to monkeypox begins with the innate immune system, which serves as the body’s first line of defense against infections. The innate immune system is composed of various cells and proteins that recognize and respond to pathogens in a non-specific manner. When MPXV enters the body, it is detected by pattern recognition receptors (PRRs) on the surface of innate immune cells, such as macrophages, dendritic cells, and natural killer (NK) cells.
These receptors recognize conserved molecular patterns on the surface of the virus, triggering an immediate immune response. One of the key responses is the production of type I interferons (IFNs), signaling proteins that play a critical role in controlling viral infections. Interferons activate antiviral defenses in neighboring cells, limiting the spread of the virus and buying time for the adaptive immune system to mount a more specific response.
Macrophages and dendritic cells are particularly important in the innate response to MPXV. These cells engulf and destroy the virus through a process called phagocytosis. Dendritic cells also act as messengers between the innate and adaptive immune systems. After capturing viral particles, they travel to the lymph nodes, where they present pieces of the virus (antigens) to T cells, initiating the adaptive immune response.
The Adaptive Immune Response: Targeting the Virus
The adaptive immune response is more specialized and takes longer to develop than the innate response. It is characterized by the activation of T cells and B cells, which work together to eliminate the virus and provide long-term immunity.
T Cells and Their Role in Fighting Monkeypox
T cells are a type of white blood cell that plays a central role in the adaptive immune response. They are divided into two main types: helper T cells (CD4+ T cells) and cytotoxic T cells (CD8+ T cells). Helper T cells assist in orchestrating the immune response by activating other immune cells, while cytotoxic T cells directly kill infected cells.
During a monkeypox infection, dendritic cells present viral antigens to T cells in the lymph nodes. This interaction activates the T cells, causing them to proliferate and differentiate into effector cells. CD8+ cytotoxic T cells then seek out and destroy cells infected with MPXV, reducing the viral load in the body and preventing the virus from spreading further.
Research has shown that during monkeypox infection, there is a significant increase in the number of CD8+ T cells, indicating that the body is mounting a robust immune response. These cells are crucial for controlling the infection, as they can recognize and eliminate infected cells before the virus has a chance to replicate and spread.
The Role of B Cells and Antibodies
B cells are another critical component of the adaptive immune system. When activated by helper T cells, B cells differentiate into plasma cells, which produce antibodies specific to the monkeypox virus. These antibodies circulate in the bloodstream, binding to viral particles and neutralizing them, preventing the virus from infecting new cells.
Antibodies can also mark viral particles for destruction by other immune cells, such as macrophages. This process, known as opsonization, enhances the efficiency of the immune response and helps to clear the virus from the body.
Importantly, the production of antibodies provides long-term immunity against MPXV. Memory B cells, a subset of B cells, remain in the body after the infection has been cleared. These cells "remember" the virus and can quickly produce antibodies if the person is exposed to MPXV again in the future, providing protection against reinfection.
The Role of Natural Killer Cells
Natural killer (NK) cells are a part of the innate immune system but play a critical role in bridging the innate and adaptive immune responses. NK cells are particularly important during the early stages of infection, as they can recognize and kill cells infected with MPXV without the need for prior exposure to the virus.
During a monkeypox infection, NK cells are activated by cytokines, signaling molecules produced by infected cells and other immune cells. Once activated, NK cells release cytotoxic granules that induce apoptosis (programmed cell death) in infected cells, limiting the spread of the virus. NK cells also produce cytokines such as interferon-gamma (IFN-γ), which further enhances the antiviral response and helps to recruit other immune cells to the site of infection.
Recent studies have highlighted the importance of NK cells in controlling monkeypox infection. Researchers have observed that during the course of the infection, there is a temporary reduction in the number of NK cells, followed by a significant expansion as the immune system ramps up its response. This pattern suggests that NK cells play a crucial role in the early containment of the virus, while other components of the immune system take over later in the infection.
 The immunopathogenesis of Mpox (Monkeypox) infections
Immune Evasion and Challenges in Fighting Monkeypox
The immunopathogenesis of Mpox (Monkeypox) infections
Immune Evasion and Challenges in Fighting Monkeypox
Despite the effectiveness of the immune system in combating monkeypox, the virus has developed several strategies to evade immune detection and suppression. MPXV encodes a variety of proteins that can interfere with the host’s immune response, making it more challenging for the body to clear the infection.
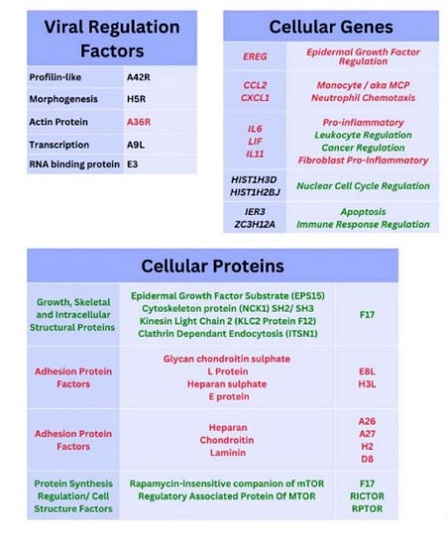
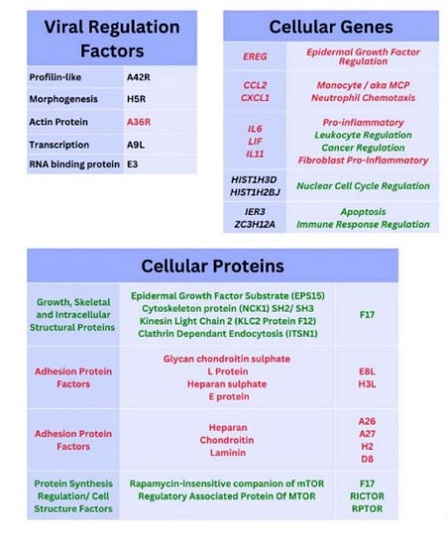
One of the key strategies employed by MPXV is the production of proteins that inhibit the action of interferons. For example, the E3L protein binds to double-stranded RNA (a viral replication intermediate) and prevents its recognition by cellular sensors that would otherwise trigger an interferon response. Additionally, MPXV produces proteins that can block the activation of natural killer cells and cytotoxic T cells, hindering their ability to kill infected cells.
Another challenge in fighting monkeypox is the potential for the virus to suppress the expression of major histocompatibility complex (MHC) molecules on the surface of infected cells. MHC molecules are essential for presenting viral antigens to T cells. If MPXV can downregulate MHC expression, it can effectively hide from the immune system, allowing the virus to persist in the host.
These immune evasion tactics underscore the importance of continued research into the immunology of monkeypox. By understanding how the virus interacts with the immune system, scientists can develop more effective vaccines and therapies that can overcome these challenges and provide better protection against the virus.
The Future of Immunology Research in Monkeypox
Ongoing research into the immune response to monkeypox is crucial for the development of new and improved vaccines and treatments. One area of focus is the identification of specific viral proteins that could serve as targets for vaccines. For example, the A42R protein has been identified as a potential vaccine target due to its role in immune activation and its high level of conservation across different strains of MPXV.
Additionally, researchers are exploring the use of immunomodulatory therapies that can enhance the body’s natural immune response to MPXV. These therapies could include cytokine treatments that boost the activity of T cells and NK cells, or monoclonal antibodies that neutralize viral particles and prevent infection.
Another promising avenue of research is the development of peptide-based vaccines that target specific epitopes on the virus. These vaccines could be designed to elicit a strong and durable immune response, providing long-lasting protection against monkeypox.
As the understanding of monkeypox immunology continues to evolve, it will be essential to translate these findings into practical applications that can benefit public health. By harnessing the power of the immune system, researchers hope to develop effective strategies to prevent and treat monkeypox, ultimately reducing the impact of this virus on global health.
Vaccines and Treatments: What Are the Options?
Vaccination remains one of the most effective ways to prevent monkeypox. The smallpox vaccine, which was instrumental in eradicating smallpox, also provides some protection against monkeypox. However, with the cessation of smallpox vaccination programs following the eradication of the disease, younger generations are particularly vulnerable to monkeypox.
Currently, there are three main vaccines used against monkeypox: ACAM2000®, JYNNEOS™, and IMVAMUNE. These vaccines are based on modified vaccinia virus strains and have shown varying degrees of effectiveness against monkeypox. Studies suggest that these vaccines offer protection ranging from 58% to 89%, depending on the specific vaccine and the population studied.
In addition to vaccines, antiviral treatments are also being explored. Tecovirimat, also known as TPOXX®, is an antiviral drug that targets the F13L protein, a key component of the monkeypox virus. Tecovirimat has been shown to be effective in treating monkeypox in animal models, and it has received approval for use in treating smallpox. Brincidofovir, another antiviral drug, is also being investigated for its potential to treat monkeypox, although more research is needed to confirm its efficacy.
The Importance of Continued Research and Surveillance
The ongoing research into monkeypox is vital for improving our understanding of the virus and developing effective countermeasures. The spread of monkeypox to non-endemic regions highlights the need for global surveillance and cooperation in monitoring and controlling the virus.
The researchers involved in this study emphasize the importance of continued vigilance, particularly in light of the potential for zoonotic transmission from animals to humans. They also stress the need for further research into the immune response to monkeypox, as well as the development of more effective vaccines and treatments.
While the Mpox virus may not be as deadly as smallpox, it still poses a significant public health threat, particularly in populations with limited access to healthcare and vaccination.
In conclusion, the fight against monkeypox is far from over. Continued research, vaccination, and public awareness are essential to preventing the spread of this virus and protecting global health. The lessons learned from past outbreaks, combined with modern scientific advances, will be crucial in managing and ultimately overcoming the threat of monkeypox.
The study findings were published on a preprint server and is currently being peer reviewed.
https://www.preprints.org/manuscript/202307.0673/v2
For the latest
Mpox News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-mpox-virus-can-survive-in-scabs-for-months-or-even-years-says-u-s-department-of-homeland-security-report
https://www.thailandmedical.news/news/new-insights-into-understanding-mpox-s-evasion-of-the-immune-system