Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 04, 2024 1 year, 1 month, 1 week, 3 days, 3 hours, 21 minutes ago
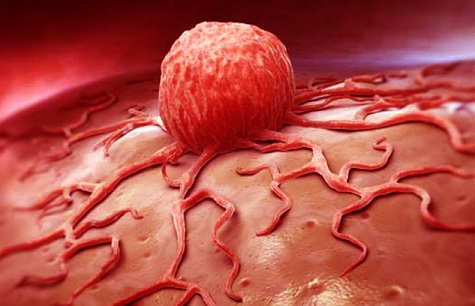
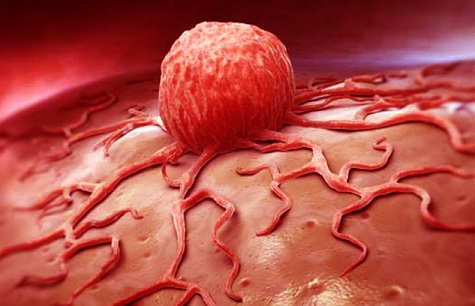
Medical News: Researchers from prestigious institutions, including Martin Luther University Halle-Wittenberg-Germany, the University of Eastern Finland, Charité in Berlin-germany, and Helmholtz-Zentrum Dresden-Rossendorf-Germany, have unveiled new insights into the angiotensin-converting enzyme 2 (ACE2). This receptor, vital for SARS-CoV-2 entry into cells, also plays significant roles in tumor biology and immune system modulation. By examining RNA sequencing data from tumor tissues, adjacent tissues, and COVID-19 patient blood samples, the study sheds light on how ACE2 alters immune responses and what this means for cancer patients, particularly during the COVID-19 pandemic.
 ACE2 Role in Tumors and COVID-19 Explored
ACE2 Role in Tumors and COVID-19 Explored
ACE2 has been a focal point of research since the onset of the COVID-19 pandemic. It serves as a gateway for the virus and influences immune responses and cellular processes in various organs. The study highlights that ACE2 expression is not only critical for understanding viral infections but also offers insights into its impact on tumors and cancer immunotherapy.
How ACE2 Interacts with Immune Responses
The study's findings underscore the significant role of ACE2 in modulating immune pathways. Researchers employed advanced techniques, including quantitative polymerase chain reaction (qPCR), Western blotting, RNA sequencing, and in silico data analysis, to investigate these dynamics.
High ACE2 expression (referred to as ACE2high) was linked to an upregulation of critical immune molecules like HLA class I and programmed death-ligand 1 (PD-L1). These molecules are central to immune checkpoint inhibitors, a modern approach to cancer therapy. The findings suggest that ACE2high cells can enhance immune cell migration and apoptosis while influencing the release of cytokines, the signaling molecules that mediate immune responses.
This
Medical News report provides a detailed analysis of how ACE2 expression in tumor and endothelial cells affects the tumor microenvironment, shaping immune responses and potentially altering the efficacy of cancer treatments.
Key Findings of the Study
The research uncovered several groundbreaking insights into ACE2's role in immune modulation:
-Immune Pathway Activation: ACE2high cells showed increased activity in pathways related to interferon signaling and antigen processing. These pathways are critical for enabling the immune system to identify and eliminate cancerous or infected cells effectively.
-Altered Cytokine Profiles: The study identified changes in cytokine secretion in ACE2high cells. For instance, IL-2 levels, which enhance adaptive immunity, were elevated, while IL-10, known for its anti-inflammatory properties, also showed increased activity. These findings demonstrate ACE2's role in modulating both pro-inflammatory and anti-inflammatory responses.
-Impact on Immune Cells: Co-cultures of ACE2high tumor
cells with immune cells revealed enhanced infiltration and apoptosis of immune cells. These interactions suggest that ACE2 expression can influence the tumor's immune microenvironment, potentially affecting disease progression and treatment responses.
-PD-L1 Expression and Immunotherapy: The study observed higher PD-L1 expression in ACE2high cells. PD-L1 is a key target for immune checkpoint inhibitors, and its upregulation could impact the efficacy of therapies designed to boost anti-tumor immune responses.
-Relevance to COVID-19: Data from COVID-19 patients showed that ACE2 expression correlates with increased interferon signaling and immune activation. These findings highlight the complex interplay between viral infections and immune regulation in cancer patients.
Possible Therapeutic Approaches
Given the multifaceted role of ACE2, the study proposes several therapeutic strategies to address its effects in cancer and COVID-19:
-Targeting the ACE2-PD-L1 Axis
The ACE2-induced upregulation of PD-L1 offers a promising therapeutic target. By inhibiting PD-L1, immune checkpoint inhibitors like nivolumab or pembrolizumab could be more effective in restoring T-cell activity and enhancing anti-tumor immunity in ACE2high patients. This approach could be particularly beneficial for cancer patients affected by COVID-19, where immune modulation is critical.
-Modulating Cytokine Responses
The study's findings on altered cytokine profiles suggest that therapies targeting specific cytokines, such as IL-10 inhibitors or IL-2 boosters, could help balance pro-inflammatory and anti-inflammatory responses. Reducing cytokine storms in COVID-19 patients with ACE2high tumors may improve outcomes.
-Personalized Immunotherapy
Given the variability in ACE2 expression among patients, personalized immunotherapy approaches could be developed. Biomarker testing for ACE2 levels and immune checkpoint molecule expression could guide treatment choices, optimizing therapeutic outcomes.
-Combination Therapies
The use of combination therapies that target ACE2 along with interferon signaling or immune checkpoint pathways could provide synergistic effects. For example, combining PD-L1 inhibitors with drugs targeting interferon pathways may enhance immune cell infiltration and reduce tumor growth.
Experimental Approaches
The study highlights the potential for using CRISPR/Cas9-mediated knockdown of ACE2 to explore its effects further. Preclinical models could validate these findings and pave the way for novel therapies targeting ACE2 and associated immune pathways.
Broader Implications for Cancer and COVID-19
This research emphasizes the dual role of ACE2 in regulating immune responses and influencing cancer progression. For cancer patients with COVID-19, ACE2 expression may serve as a biomarker to identify those at higher risk of severe outcomes. The interplay between ACE2, immune modulation, and viral infections underscores the need for integrated approaches to manage cancer and infectious diseases.
The findings suggest that high ACE2 expression could improve the efficacy of cancer immunotherapies, particularly in the context of viral infections. However, the associated risks, such as enhanced PD-L1 expression and potential immune suppression, warrant careful consideration.
Conclusions and Future Directions
This comprehensive study sheds light on the complex role of ACE2 in cancer and immune regulation. The findings highlight the potential for leveraging ACE2 pathways to enhance cancer immunotherapies and improve outcomes for patients affected by COVID-19. By targeting the ACE2-PD-L1 axis and modulating immune responses, novel therapeutic strategies could be developed to address these challenges.
Future research should focus on in vivo studies to validate these findings and explore the therapeutic potential of ACE2-targeted interventions. The development of personalized approaches, including biomarker-guided therapies and combination treatments, will be crucial for optimizing outcomes.
The study findings were published in the peer-reviewed journal: Cellular and Molecular Life Sciences.
https://link.springer.com/article/10.1007/s00018-024-05520-9
For the latest Medical Research News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/chinese-study-uncovers-impact-of-covid-19-on-cancer-progression
https://www.thailandmedical.news/news/decoding-the-role-of-p53-in-cancer
https://www.thailandmedical.news/news/covid-19-linked-to-relapse-in-blood-cancers