Nikhil Prasad Fact checked by:Thailand Medical News Jun 17, 2024 10 months, 3 days, 9 hours, 27 minutes ago
Sepsis: In a remarkable breakthrough, a clinical trial supported by the U.S. National Institutes of Health (NIH) has shown that acetaminophen, a common pain reliever, may have a powerful new use in treating sepsis. This discovery is especially promising for the most critically ill patients, indicating that acetaminophen can significantly reduce the risk of organ damage and acute respiratory distress syndrome (ARDS), potentially transforming the way sepsis is managed in hospitals.
 Acetaminophen's Potential in Sepsis Treatment
Understanding Sepsis
Acetaminophen's Potential in Sepsis Treatment
Understanding Sepsis
Sepsis is a severe and potentially life-threatening condition that occurs when the body’s response to infection triggers widespread inflammation, leading to organ dysfunction. In the worst cases, it can progress to septic shock, a dramatic drop in blood pressure that can cause lasting damage to vital organs such as the lungs, kidneys, and liver. Despite advances in medical care,
Sepsis remains a leading cause of death in hospitals, highlighting the urgent need for more effective treatments.
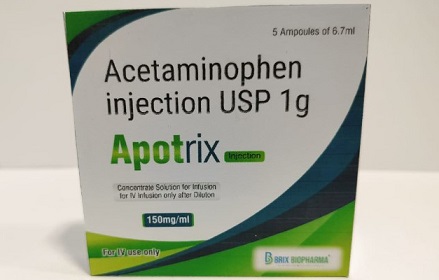
The Breakthrough Clinical Trial
From October 2021 to April 2023, researchers conducted a mid-stage clinical trial across 40 academic hospitals in the United States, enrolling 447 adults with sepsis. These patients were suffering from respiratory or circulatory organ dysfunction, making them critically ill. The participants were randomly assigned to receive either intravenous acetaminophen or a placebo every six hours for five days. The main objective was to see how many patients could survive without needing organ support, such as mechanical ventilation or kidney replacement therapy, over a period of 28 days.
Key Findings of the Study
The trial produced several noteworthy findings:
-Safety Profile: Acetaminophen was found to be safe for all patients involved in the study. There were no significant differences in adverse events, such as liver injury or low blood pressure, between the acetaminophen group and the placebo group. This finding is crucial because it suggests that acetaminophen can be administered without additional risks to patients already in critical condition.
-Reduction in Organ Injury: Patients who received acetaminophen experienced significantly lower rates of organ injury compared to those who received the placebo. This was particularly evident in the reduction of acute respiratory distress syndrome (ARDS) within the first seven days of hospital admission. ARDS is a severe condition that causes fluid to leak into the lungs, making breathing difficult and often leading to mechanical ventilation.
-Need for Assisted Ventilation: Only 8% of patients in the acetaminophen group required assisted ventilation, compared to 23% in the placebo group. This dramatic difference underscores the potential of acetaminophen to reduce the severity of respiratory complications in sepsis patients.
-Mortality Rates: A
fter 28 days, 12% of patients in the acetaminophen group had died, compared to 21% in the placebo group. Although this difference was not statistically significant, it indicates a positive trend and suggests that further research could solidify acetaminophen’s role in improving survival rates among the most critically ill sepsis patients.
The Role of Cell-Free Hemoglobin
A critical aspect of the study focused on cell-free hemoglobin; a substance released into the bloodstream when red blood cells are damaged. In sepsis, red blood cells are injured at abnormally high rates, releasing large amounts of cell-free hemoglobin. The body’s systems become overwhelmed, unable to remove this excess, which can lead to significant organ damage.
Dr Lorraine Ware, a professor of medicine at Vanderbilt University and the first author of the study, had previously shown that acetaminophen could block the harmful effects of cell-free hemoglobin on the lungs, which are at high risk of injury during sepsis. Her earlier research suggested that patients with the highest levels of cell-free hemoglobin might benefit the most from acetaminophen therapy.
Potential for Biomarker Use
The discovery of cell-free hemoglobin as a biomarker is a significant breakthrough. Biomarkers are measurable indicators of a biological condition or disease. In this case, high levels of cell-free hemoglobin could help doctors quickly identify which sepsis patients are at greatest risk for organ damage and might benefit most from acetaminophen therapy.
“One problem in critical care is that patients get sick so fast, we often don’t have time to figure out which biomarkers help predict which therapy could give the best outcome,” said Dr Michael Matthay, a professor of medicine and anesthesia at the University of California, San Francisco, and the senior author of the study. “These findings underscore the potential therapeutic value of using a biomarker to find the right treatment when patients need it the most.”
Detailed Analysis and Future Directions
The researchers conducted a detailed analysis using data from patients with high levels of cell-free hemoglobin. They found that among these patients, acetaminophen was particularly effective. The significant reduction in the need for assisted ventilation and the positive trend in mortality rates highlight the potential of this treatment.
Despite the promising results, the study's authors emphasize that more research is needed. They plan to conduct a larger clinical trial, focusing on patients with elevated levels of cell-free hemoglobin, to validate these findings and explore the mechanisms behind acetaminophen’s protective effects in sepsis.
“While the anticipated effects of acetaminophen therapy were not realized for all sepsis patients, this study shows that it still holds promise for the most critically ill,” said Dr James Kiley, director of the Division of Lung Diseases at the National Heart, Lung, and Blood Institute, part of U.S. NIH. “More research is needed to uncover the mechanisms and validate these results.”
Dr Ware and Dr Matthay are optimistic about the future trials. They believe that focusing on the most critically ill patients, who have higher levels of cell-free hemoglobin, will provide more definitive answers and potentially lead to a new standard of care in sepsis treatment.
Conclusion
The use of acetaminophen in treating sepsis represents a potentially transformative approach, especially for those at the highest risk of severe complications. By leveraging biomarkers like cell-free hemoglobin, doctors may soon have a powerful new tool in the fight against this deadly condition. As research continues, the hope is to improve outcomes for the most vulnerable patients and offer a new ray of hope in the treatment of sepsis.
This study highlights the importance of ongoing research and the need for innovative approaches to treating complex medical conditions like sepsis. The promising results from this clinical trial could pave the way for new treatment protocols that save lives and improve the quality of care for sepsis patients worldwide.
The study findings were published in the peer reviewed journal: JAMA Network.
https://jamanetwork.com/journals/jama/article-abstract/2819082
For more about
Sepsis, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/researchers-stop-cell-suicide-that-worsens-sepsis-arthritis
https://www.thailandmedical.news/news/covid-19-clinical-care-acute-gastrointestinal-injury-occurs-in-almost-86-percent-of-critical-condition-covid-19-patients,-often-leading-to-sepsis-and-