Activation Of Type 1 Dendritic Cells CD11c+ CD141+ CLEC9A+ And Exhausted Natural Killer Cells Are Key Drivers Of Post COVID Multisystem Inflammatory Syndrome
Source: Medical News - Multisystem Inflammatory Syndrome Mar 06, 2022 3 years, 1 month, 2 weeks, 6 days, 21 minutes ago
A new study by researchers from Columbia University Medical Center-USA and University of Buffalo-USA has found that activation of Type 1 dendritic cells such as CD11c+ CD141+ and CLEC9A+m along with exhausted natural killer cells are key drivers of the Post COVID condition known as
Multisystem Inflammatory Syndrome or MIS which can affect both children (MIS-C) or adults (MIS-A). the study also found that that the cytokine interleukin-27, an inflammatory molecule, was very highly upregulated in patients with MIS.
.jpg) Graphical Abstract
Graphical Abstract
Multisystem inflammatory syndrome is an acute, febrile, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-associated syndrome, often with cardiohemodynamic dysfunction.
To date, insights into the mechanism of the condition is still not properly known.
The study team objective was to analyze immunologic features of MIS-C patients compared to febrile controls (FC).
For the study, MIS-C patients were defined by narrow criteria, including having evidence of cardiohemodynamic involvement and no macrophage activation syndrome.
Samples were collected from 8 completely treatment-naive patients with MIS-C (SARS-CoV-2 serology positive), 3 patients with unclassified MIS-C–like disease (serology negative), 14 FC, and 5 MIS-C recovery (RCV). Three healthy controls (HCs) were used for comparisons of normal range.
Utilizing spectral flow cytometry, the study team assessed 36 parameters in antigen-presenting cells (APCs) and 29 in T cells.
The team used biaxial analysis and uniform manifold approximation and projection (UMAP).
The study found significant elevations in cytokines including CXCL9, M-CSF, and IL-27 were found in MIS-C compared to FC. Classic monocytes and type 2 dendritic cells (DCs) were downregulated (decreased CD86, HLA-DR) versus HCs; however, type 1 DCs (CD11c+CD141+CLEC9A+) were highly activated in MIS-C patients versus FC, expressing higher levels of CD86, CD275, and atypical conventional DC markers such as CD64, CD115, and CX3CR1. CD169 and CD38 were upregulated in multiple monocyte subtypes.
CD56dim/CD57−/KLRGhi/CD161+/CD38− natural killer (NK) cells were a unique subset in MIS-C versus FC without macrophage activation syndrome.
The study findings showed that complex cytokine signaling, type 1 DC activation and NK dysregulation are key features in the pathophysiology of MIS-C. NK cell findings may suggest a relationship with macrophage activation syndrome, while type 1 DC upregulation implies a role for antigen cross-presentation.
Please help support this website by making a donation not only for the sustainability of the website but also for all our research and community initiatives. We are not funded by any entities and really need help. Your help not only saves lives directly but also indirectly.
93);">https://www.thailandmedical.news/p/sponsorship
The study findings were published in the peer reviewed Journal of Allergy and Clinical Immunology.
https://www.jacionline.org/article/S0091-6749(21)01627-4/fulltext
The study findings identified unique features of MIS-C, a rare but potentially deadly complication of COVID in children, that suggest how the syndrome gets started. The same syndrome can also affect adults.
The research, led by Dr Mark Gorelik, MD, assistant professor of pediatrics, and Dr Robert Winchester, MD, professor of medicine, pathology & cell biology, and pediatrics, is the first study to identify the factors that trigger this condition.
The study findings may lead to faster diagnosis and better treatment of MIS-C (also known as multisystem inflammatory syndrome in children) and also MIS-A. (multisystem inflammatory syndrome in adults).
Dr Gorelik told Thailand
Medical News, "One of the major unanswered questions about MIS-C is how, immunologically, the disease evolves from the initial infectious episode to the final, immune-mediated assault. One way to study this could be to identify what is unique about the inflammatory/immunologic response in MIS-C."
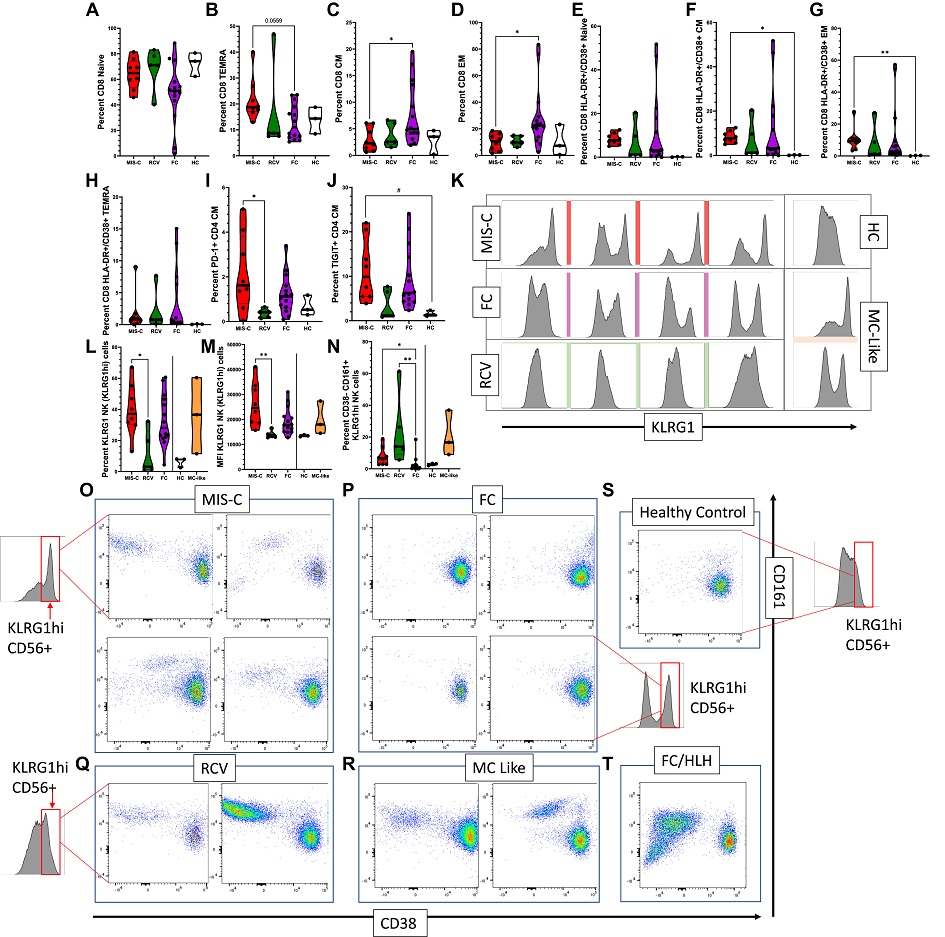 Expression of markers on the T and NK cell compartment. (A-D) Percentage of T-cell subtypes in patients with MIS-C versus FC and RCV. (E-H) Percentage of CD38+HLA-DR+ T-cell subsets in patients with MIS-C versus FC and RCV. (I, J) Percentage TIGIT+ and PD-1+ in CD4 T-cell CM. (K) Histogram showing upregulated KLRG1 in MIS-C patients versus RCV, HC, and FC subjects. (L) Percentage of KLRG1hi NK cells seen in MIS-C versus RCV and FC patients. (M) MFI in MIS-C patients versus RCV and FC patients; MIS-C–like patients are shown for comparison but statistical analysis not performed (line indicating where no statistical analysis performed); (N) Percentage of KLRG1hi, CD38−CD161+ NK cells in MIS-C versus RCV and FC patients, MIS-C–like patients again included. (O-T) Biaxial analysis of CD38 and CD161 expression in KLRG1hi NK cells from MIS-C, FC, RCV, HC, and MIS-C–like subjects and in a FC with HLH. KLRG1hi NK cells were gated in all subgroups from the same KLRG1hi region (red box, demonstrated visually on the graph in some of the subgroups for explanation; the same region was sampled in the FC/HLH and the MIS-C–like patients). ∗∗P < .01, ∗P < .05 (with multiple comparisons, Kruskal Wallis test with Dunn correction), #P < .05 (single comparisons, Mann-Whitney U test without correction); when no comparison bar is shown with HCs, a statistical test was not performed, and HC information is shown to represent an index of normal range. HCs and MIS-C–like patients included for (M) and (N). CM, Central memory; EM, effector memory; MFI, mean fluorescence index.
Expression of markers on the T and NK cell compartment. (A-D) Percentage of T-cell subtypes in patients with MIS-C versus FC and RCV. (E-H) Percentage of CD38+HLA-DR+ T-cell subsets in patients with MIS-C versus FC and RCV. (I, J) Percentage TIGIT+ and PD-1+ in CD4 T-cell CM. (K) Histogram showing upregulated KLRG1 in MIS-C patients versus RCV, HC, and FC subjects. (L) Percentage of KLRG1hi NK cells seen in MIS-C versus RCV and FC patients. (M) MFI in MIS-C patients versus RCV and FC patients; MIS-C–like patients are shown for comparison but statistical analysis not performed (line indicating where no statistical analysis performed); (N) Percentage of KLRG1hi, CD38−CD161+ NK cells in MIS-C versus RCV and FC patients, MIS-C–like patients again included. (O-T) Biaxial analysis of CD38 and CD161 expression in KLRG1hi NK cells from MIS-C, FC, RCV, HC, and MIS-C–like subjects and in a FC with HLH. KLRG1hi NK cells were gated in all subgroups from the same KLRG1hi region (red box, demonstrated visually on the graph in some of the subgroups for explanation; the same region was sampled in the FC/HLH and the MIS-C–like patients). ∗∗P < .01, ∗P < .05 (with multiple comparisons, Kruskal Wallis test with Dunn correction), #P < .05 (single comparisons, Mann-Whitney U test without correction); when no comparison bar is shown with HCs, a statistical test was not performed, and HC information is shown to represent an index of normal range. HCs and MIS-C–like patients included for (M) and (N). CM, Central memory; EM, effector memory; MFI, mean fluorescence index.
It should be noted that although numerous other studies have looked at the immune and inflammatory response in MIS-C patients, most have looked at patients after initiation of treatment and made comparisons with healthy controls.
Dr Gorelik further added, "To us, comparisons to healthy controls would not differentiate the basic inflammatory response to infection from the unique features of MIS-C, and, of course, treatment would muddy the waters."
The study team compared eight MIS-C patients with 14 patients with other febrile infections, by looking at the array of immune cells and responses in blood samples taken at the very first encounter with care in the emergency department, before treatments were initiated.
A key clue to what causes MIS-C may lie in the different immune cells found in MIS-C patients compared with other patients.
Dr Winchester added, "Only some cells were activated, which suggests that these cells are mistakenly directing the immune system to attack blood vessels in the body that had been damaged by the virus. These cells are drawn to the blood vessels because of the presence of the virus, but they appear to misidentify the culprit when they alert the rest of the immune system."
Multisystem inflammatory syndrome in children or MIS-C also appears to drive patients' natural killer cells, another type of immune cell to exhaustion.
Dr Winchester said, "They get to the point where they are no longer able to carry out their function properly. This is seen in some other inflammatory diseases and may offer a clue to treatment similar to those diseases."
Importantly, another key finding from the study may give doctors an easier way to diagnose MIS-C, which can be hard to distinguish from other syndromes. This finding is that interleukin-27, an inflammatory molecule, was very highly upregulated in patients with MIS-C but not in other febrile children.
Dr Gorelik further added, "This cytokine is poorly understood but has been associated with increased mortality in patients with serious blood infection or sepsis. If validated, these study findings may allow researchers to run a simple, easily available test to readily confirm MIS-C in patients when they are in the emergency department."
The study team postulates that MIS-C and adult COVID-19 infection may be more similar than is currently believed.
Dr Gorelik commented, "We noticed that several of our findings have also been reported in studies of adult patients with severe, late-stage COVID-19 infection. Perhaps, and this is highly speculative…what is unique to children is the ability to handle the initial viral infection more efficiently, and then a month or so later they develop MIS-C. In contrast, adults are not able to suppress the initial viral infection. And then secondarily, in severe cases, a serious MIS-C-like immune response develops. In both adults and children, however, this second phase immune signature appears quite similar."
The study team did however warn of certain study limitations… mainly, “There was lack of more extensive markers to further evaluate NK cell activity, such as perforin, NKD2D, and CD16. This was the result of our expectation that the primary pathology would be found in the T-cell compartment, and although T-cell abnormalities were found in our data, we were somewhat surprised by the evident NK cell findings. Future studies will more comprehensively analyze the changes in these cells.”
Please help support this website by making a donation not only for the sustainability of the website but also for all our research and community initiatives. We are not funded by any entities and really need help. Your help not only saves lives directly but also indirectly.
https://www.thailandmedical.news/p/sponsorship
For more on
Post COVID Multisystem Inflammatory Syndrome (MIS), keep on logging to Thailand Medical News.
.jpg) Graphical Abstract
Graphical Abstract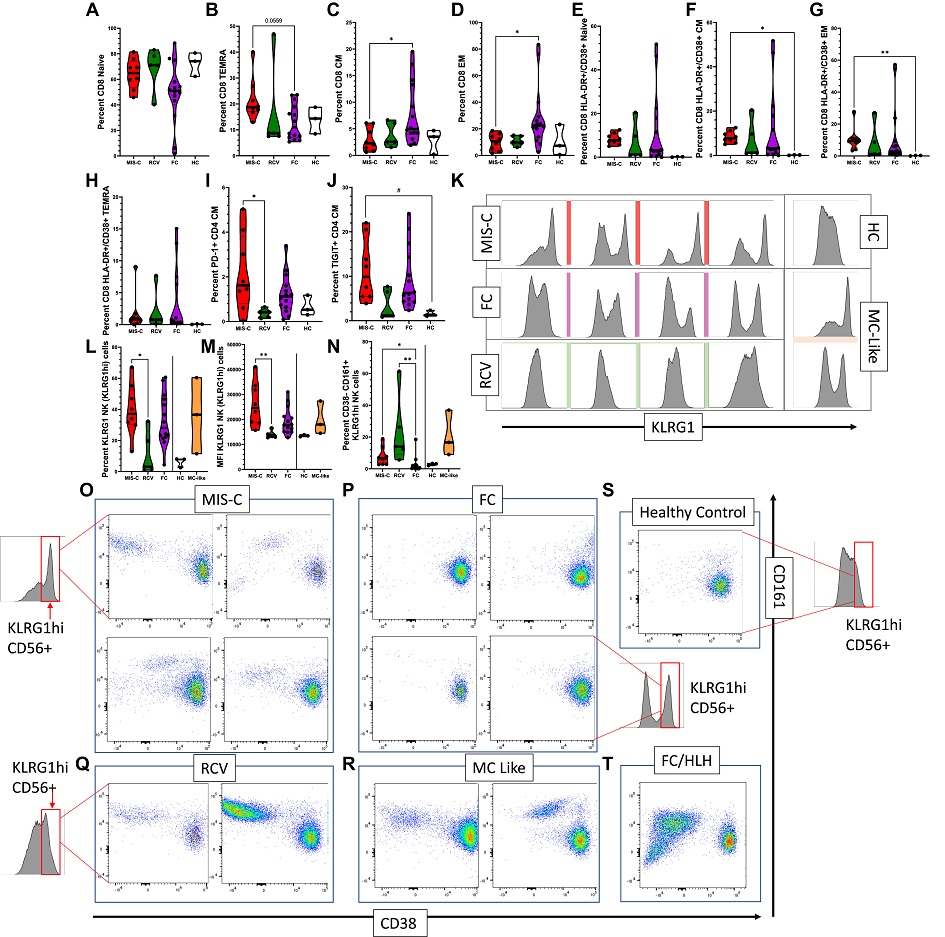 Expression of markers on the T and NK cell compartment. (A-D) Percentage of T-cell subtypes in patients with MIS-C versus FC and RCV. (E-H) Percentage of CD38+HLA-DR+ T-cell subsets in patients with MIS-C versus FC and RCV. (I, J) Percentage TIGIT+ and PD-1+ in CD4 T-cell CM. (K) Histogram showing upregulated KLRG1 in MIS-C patients versus RCV, HC, and FC subjects. (L) Percentage of KLRG1hi NK cells seen in MIS-C versus RCV and FC patients. (M) MFI in MIS-C patients versus RCV and FC patients; MIS-C–like patients are shown for comparison but statistical analysis not performed (line indicating where no statistical analysis performed); (N) Percentage of KLRG1hi, CD38−CD161+ NK cells in MIS-C versus RCV and FC patients, MIS-C–like patients again included. (O-T) Biaxial analysis of CD38 and CD161 expression in KLRG1hi NK cells from MIS-C, FC, RCV, HC, and MIS-C–like subjects and in a FC with HLH. KLRG1hi NK cells were gated in all subgroups from the same KLRG1hi region (red box, demonstrated visually on the graph in some of the subgroups for explanation; the same region was sampled in the FC/HLH and the MIS-C–like patients). ∗∗P < .01, ∗P < .05 (with multiple comparisons, Kruskal Wallis test with Dunn correction), #P < .05 (single comparisons, Mann-Whitney U test without correction); when no comparison bar is shown with HCs, a statistical test was not performed, and HC information is shown to represent an index of normal range. HCs and MIS-C–like patients included for (M) and (N). CM, Central memory; EM, effector memory; MFI, mean fluorescence index.
Expression of markers on the T and NK cell compartment. (A-D) Percentage of T-cell subtypes in patients with MIS-C versus FC and RCV. (E-H) Percentage of CD38+HLA-DR+ T-cell subsets in patients with MIS-C versus FC and RCV. (I, J) Percentage TIGIT+ and PD-1+ in CD4 T-cell CM. (K) Histogram showing upregulated KLRG1 in MIS-C patients versus RCV, HC, and FC subjects. (L) Percentage of KLRG1hi NK cells seen in MIS-C versus RCV and FC patients. (M) MFI in MIS-C patients versus RCV and FC patients; MIS-C–like patients are shown for comparison but statistical analysis not performed (line indicating where no statistical analysis performed); (N) Percentage of KLRG1hi, CD38−CD161+ NK cells in MIS-C versus RCV and FC patients, MIS-C–like patients again included. (O-T) Biaxial analysis of CD38 and CD161 expression in KLRG1hi NK cells from MIS-C, FC, RCV, HC, and MIS-C–like subjects and in a FC with HLH. KLRG1hi NK cells were gated in all subgroups from the same KLRG1hi region (red box, demonstrated visually on the graph in some of the subgroups for explanation; the same region was sampled in the FC/HLH and the MIS-C–like patients). ∗∗P < .01, ∗P < .05 (with multiple comparisons, Kruskal Wallis test with Dunn correction), #P < .05 (single comparisons, Mann-Whitney U test without correction); when no comparison bar is shown with HCs, a statistical test was not performed, and HC information is shown to represent an index of normal range. HCs and MIS-C–like patients included for (M) and (N). CM, Central memory; EM, effector memory; MFI, mean fluorescence index.