Another Study Findings Adds To The Increasing Evidence That SARS-CoV-2 Infection Increases Risk Of Brain Degeneration That Will Lead To Parkinson's Disease!
Source: Medical News - NeuroCOVID May 19, 2022 2 years, 11 months, 1 week, 1 hour, 9 minutes ago
NeuroCOVID: A new study by researchers from the Institute for Neuroscience at Thomas Jefferson University- Philadelphia, East Carolina University and New York University has discovered findings that adds to the growing evidence that SARS-CoV-2 infections, irrespective of the nature of the infection ie whether asymptomatic or symptomatic, mild, moderate or severe, will lead to increased risk of brain degeneration that will ultimately lead to Parkinson’s Disease.
Already Thailand Medical News had covered numerous research studies in the past that indicates that many Post COVID individuals are likely to develop Parkinson’s disease due to a number of pathways after by the virus and proteins triggered in the process.
https://www.thailandmedical.news/news/study-uncovers-that-sars-cov-2-n-proteins-are-able-to-enter-stress-granules-and-cause-amyloid-aggregation,-leading-to-various-neurodegenerative-issues
https://www.thailandmedical.news/news/great-news-university-of-oxford-study-shows-that-even-mild-sars-cov-2-infections-can-result-in-brain-changes-and-cognitive-decline
https://www.thailandmedical.news/news/university-of-oklahoma-study-discovers-how-the-polypeptide-sk9-from-the-envelope-protein-of-sars-cov-2-causes-parkinson-s-disease
https://www.thailandmedical.news/news/two-new-studies-shows-sars-cov-2-infections-will-ultimately-lead-to-enhanced-risk-of-developing-neurodegenerative-diseases-like-alzheimer-s-or-parkins
https://www.thailandmedical.news/news/breaking-australian-study-discovers-that-sars-cov-2-promotes-microglial-nlrp3-inflammasome-activation-via-spike-ace2-receptor-interaction
https://www.thailandmedical.news/news/read-study-shows-sars-cov-2-n-protein-interacts-with-host-s-synuclein-proteins,-promoting-accelerated-amyloid-formation-and-parkinson-s-disease
https://www.thailandmedical.news/news/breaking-sars-cov-2-contains-amyloidogenic-peptide-fragments-that-are-neurotoxic-to-human-hosts
ews/breaking-sars-cov-2-spike-proteins-bind-to-brain-s-mao-enzymes-causing-neurological-issues-binding-affinity-is-enhanced-in-some-emerging-variants">https://www.thailandmedical.news/news/breaking-sars-cov-2-spike-proteins-bind-to-brain-s-mao-enzymes-causing-neurological-issues-binding-affinity-is-enhanced-in-some-emerging-variants
https://www.thailandmedical.news/news/long-covid-19-news-one-in-three-infected-with-sars-cov-2-will-experience-neurological-or-psychiatric-issues-months-later-many-will-get-strokes
https://www.thailandmedical.news/news/study-indicates-that-even-those-with-mild-or-asymptomatic-covid-19-can-develop-brain-inflammation-and-other-neurological-conditions-in-long-term
https://www.thailandmedical.news/news/viral-persistence-georgia-state-university-study-indicates-that-sars-cov-2-may-hide-in-the-brain-and-cause-relapses-in-recovered-patients
https://www.thailandmedical.news/news/breaking-virus-news-documented-cases-emerging-showing-that-covid-19-infection-could-lead-to-parkinson-s-disease
https://www.thailandmedical.news/news/neurologists-in-a-collaborative-study-identify-stages-of-brain-damage-caused-by-covid-19-and-warns-of-future-issues-in-recovered-patients
https://www.thailandmedical.news/news/must-read-covid-19-effects-study-says-that-covid-19-could-lead-to-increase-in-parkinson-s-disease-among-those-infected
https://www.thailandmedical.news/news/warning-researchers-say-that-a-host-of-neuropsychiatric-problems-may-emerge-in-covid-19-recovered-patients-or-in-those-that-are-asymptomatic
https://www.thailandmedical.news/news/breaking-news-more-cases-emerging-of-covid-19-affecting-the-brains-in-patients
https://www.thailandmedical.news/news/breaking-news-coronavirus-can-also-attack-the-nervous-system,-causing-neurological-conditions-and-even-viral-encephalitis
The phenomena of viral induction of neurological syndromes has been a concern since parkinsonian-like features were observed in patients diagnosed with encephalitis lethargica subsequent to the 1918 influenza pandemic. Given the similarities in the systemic responses following SARS-CoV-2 infection with those observed after pandemic influenza, there is a question if a similar syndrome of post-encephalic parkinsonism could follow COVID-19 infection.
The
NeuroCOVID study team wanted to determine if prior infection with SARS-CoV-2 increased sensitivity to a mitochondrial toxin known to induce parkinsonism.
For the study, K18-hACE2 mice were infected with SARS-CoV-2 to induce mild to moderate disease. After 38 days recovery, mice were administered a non-lesion inducing dose of the parkinsonian toxin MPTP and euthanized 7 days later. Subsequent neuroinflammation and SNpc dopaminergic neuron loss was determined and compared to SARS-CoV-2 or MPTP alone.
The study findings showed that K18-hACE2 mice infected with SARS-CoV-2 or MPTP showed no SNpc DA neuron loss following MPTP.
However, in mice infected and recovered from SARS-CoV-2 infection, MPTP induced a 23% or 19% greater loss of SNpc dopaminergic neurons than SARS-CoV-2 or MPTP, respectively (p < 0.05). Examination of microglial activation showed a significant increase in the number of activated microglia in both the SNpc and striatum of the SARS-CoV-2 + MPTP group compared to SARS-CoV-2 or MPTP alone.
The study findings have important implications for long-term public health, given the number of people that have survived SARS-CoV-2 infection as well as for future public policy regarding infection mitigation. However, it will be critical to determine if other agents known to increase risk of PD also have synergistic effects with SARS-CoV-2 and are abrogated by vaccination.
The study findings were published in the peer reviewed journal: Movement Disorders (The Official Journal Of The International Parkinson Movement Disorder Society.)
https://movementdisorders.onlinelibrary.wiley.com/doi/10.1002/mds.29116
Doctors around the world have observed many neurological symptoms including brain fog, headaches, insomnia in COVID-19 patients.
It should however be noted that neurological sequelae after a viral infection is not new, in fact, following the 1918 influenza pandemic, it took almost a decade for patients to present with the neurological syndrome called "post-encephalic parkinsonism."
.jpg)
However, the mechanisms by which viruses impact the brain is poorly understood.
The study team showed in this new study performed in mice, that the SARS-CoV-2 virus responsible for the COVID-19 pandemic could increase the risk of brain degeneration seen in Parkinson's disease.
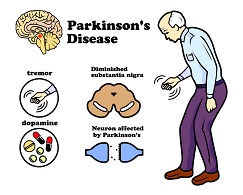
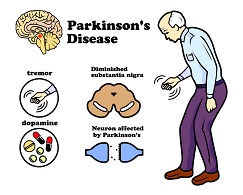
Typically, Parkinson's is a rare disease that affects 2% of the population above 55 years. However, the current COVID-19 crisis with billions of people already exposed to the virus is causing a panic among the medical community as Parkinson’s Disease could be the next global health issue that will have an impact on public healthcare.
Hence understanding how coronavirus impacts the brain can help us prepare for the long-term consequences of this pandemic.
This study builds on previous evidence from the lab of Dr Richard Smeyne, PhD, Director of the Jefferson Comprehensive Parkinson's Disease and Movement Disorder Center at the Vickie and Jack Farber Institute for Neuroscience and first author of the study. That previous study findings showed that viruses can make brain cells or neurons more susceptible to damage or death.
The researchers in that earlier study, found that mice infected with the H1N1 strain of influenza responsible for the 2009 flu pandemic, were more susceptible to MPTP, a toxin that is known to induce some of the characteristic features of Parkinson's: primarily the loss of neurons expressing the chemical dopamine and increased inflammation in the basal ganglia, a brain region that is critical for movement.
These findings in mice were later confirmed in humans by researchers in Denmark, who showed that influenza nearly doubled the risk of developing Parkinson's disease within 10 years after initial infection.
The current study team used mice that were genetically engineered to express the human ACE-2 receptor, which the SARS-CoV-2 virus uses to gain access to the cells in our airway. These mice were infected with SARS-CoV-2 and allowed to recover. Importantly, the dose chosen in this study corresponds to moderate COVID-19 infection in humans, with around 80% of the infected mice surviving. Thirty-eight days after the surviving animals recovered, one group was injected with a low dose of MPTP that would not normally cause any loss of neurons. The control group was given saline. Two weeks later, the animals were sacrificed and their brains examined.
The study team found that COVID-19 infection alone had no effect on the dopaminergic neurons in the basal ganglia.
However, mice that were given the low dose of MPTP after recovering from infection exhibited the classic pattern of neuron loss seen in Parkinson's disease. This increased sensitivity after COVID-19 infection was similar to what was seen in the influenza study; this suggests that both viruses could induce an equivalent increase in risk for developing Parkinson's.
Dr Smeyne told Thailand
Medical News, "We think about a 'multi-hit' hypothesis for Parkinson's ie the virus itself does not kill the neurons, but it does makes them more susceptible to a 'second hit', such as a toxin or bacteria or even an underlying genetic mutation.”
Thailand
Medical News would like to add that perhaps even reinfections with various variants of the SARS-CoV-2 could also possibility have a similar effect!
It has been found that both influenza and SARS-CoV2 have been found to cause a "cytokine storm" or an overproduction of pro-inflammatory chemicals. These chemicals can cross the blood-brain barrier and activate the brain's immune cells – microglia.
The study team found increased numbers of activated microglia in the basal ganglia of mice that recovered from SARS-CoV2 and received MPTP. While the mechanism is not fully understood, the study team believe the increased microglia inflame the basal ganglia and cause cellular stress. This then lowers the neurons' threshold to withstand subsequent stress.
Dr Peter Schmidt, PhD, a neuroscientist from New York University and co-researcher of the study added, "We were concerned about the long-term consequences of viral infection. Dr Smeyne is a leader in this area of research and Jefferson was the ideal site to perform the analysis."
The study team is planning to determine whether vaccines can mitigate the experimental increase in Parkinson's pathology linked to prior SARS-CoV-2 infection. They are also testing other variants of the virus, as well as doses that correspond to milder cases in humans.
Although their findings adds to the growing evidence of a link between the coronavirus and Parkinson's disease, Dr Smeyne says there are some important caveats.
He explained, "First of all, this is preclinical work. It is too soon to say whether we would see the same thing in humans, given that there seems to a 5 to 8 year lag between any changes in clinical manifestation of Parkinson's in humans."
However, this lag, he says could be used to our advantage. "If it does turn out that COVID-19 increases the risk of Parkinson's, it will be a major burden on our society and healthcare system. But we can anticipate that challenge by advancing our knowledge of potential 'second hits' and mitigating strategies."
For the latest on
NeuroCOVID, keep on logging to Thailand Medical News.
.jpg)