Antibodies Elicited By Inactivated Viral Vaccines Against SARS-CoV-2 Nsp3 Found To Also Target Host Muscle And Neuroglial Cells!
Nikhil Prasad Fact checked by:Thailand Medical News Team Jan 28, 2024 1 year, 2 months, 3 weeks, 6 days, 16 hours, 55 minutes ago
COVID-19 News: In the ongoing battle against the SARS-CoV-2, vaccines have played a crucial role in protecting public health and curbing the viral spread. Among the various vaccine types, inactivated viral vaccines, cost-effective and widely utilized in countries like India and China, have come under scrutiny due to the presence of non-capsid proteins that may trigger adverse immune responses.
A recent study that is featured in this
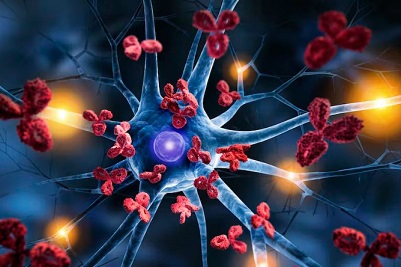
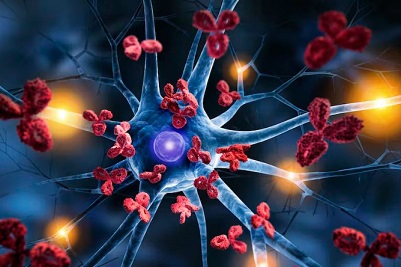
COVID-19 News article, has uncovered a concerning revelation: antibodies against the non-structural protein 3 (NSP3) of SARS-CoV-2 exhibit cross-reactivity with human muscle cells and neuroglial cells. This discovery raises questions about the potential risks associated with high antibody titers and necessitates a closer examination of inactivated viral vaccines' safety.
 Antibodies Elicited By Inactivated Viral Vaccines Against SARS-CoV-2
Antibodies Elicited By Inactivated Viral Vaccines Against SARS-CoV-2
Nsp3 Also Target Host Muscle And Neuroglial Cells
The Homology Between SARS-CoV-2 NSP3 and Human PARP14
The study, conducted by researchers from Sichuan Agricultural University, Sichuan Kelun Pharmaceutical Company Ltd, Haisco Pharmaceutical Group Company Ltd, Xijing Hospital (Medical University of the Air Force, Xi'an), and Northwest University (Xi'an), delved into the homology between the ADP-ribose-binding domains of SARS-CoV-2 NSP3 and human poly(ADP-ribose) polymerase family member 14 (PARP14). The report revealed a significant degree of homology, with core sequences sharing an identity of 32%.
The Cross-Reactivity of Antibodies
Notably, antibodies against SARS-CoV-2 NSP3 were found to bind with human PARP14 protein. However, introducing specific mutations into NSP3 significantly decreased the antibody titer against PARP14. More alarmingly, these antibodies displayed cross-reactivity with human skeletal muscle cells and astrocytes but not with human embryonic kidney 293T cells. The introduction of specific mutations into NSP3 mitigated this cross-reaction, highlighting the importance of understanding the potential consequences of these immune responses.
Implications for COVID-19 Patients
The findings suggest that individuals recovering from COVID-19 with high antibody titers against NSP3 may face elevated risks of muscular and neurological complications. This implies a potential association between NSP3-antibody-mediated autoimmune disorders and reported side effects of inactivated viral vaccines, particularly those related to the muscular and neurological systems.
The Role of NSP3 and PARP14 in COVID-19 Severity
NSP3, a vital protein in viral RNA-processing, plays a crucial role in coordinating the mammalian immune response to viral infections. The study highlights the significance of NSP3 and PARP14 as putative drug targets associated with COVID-19 severity. Macrophage activation syndrome, complicating severe COVID-19, involves the ADP-ribosylation of STAT1 by PARP14, suppressing macrophage activati
on. Understanding these molecular interactions sheds new light on potential strategies for drug development targeting SARS-CoV-2 and improving the safety of inactivated viral vaccines.
Homology Modeling and Epitope Analysis
The study employed homology modeling to analyze the peptide sequences of the macrodomains in SARS-CoV-2 NSP3 and human PARP14. The homology models, constructed using the SWISS-MODEL Workspace, provided insights into the structural similarities between the two proteins. Furthermore, the analysis of antibody epitopes revealed potential sites of interaction, with emphasis on surface accessibility.
Discussion and Future Considerations
While antibodies against SARS-CoV-2 NSP3 were found to bind human PARP14 protein, the study acknowledges that cross-reactivity with human cells requires the surface presence of PARP14. Positive controls using anti-PARP14 antibodies confirmed the surface presence of PARP14 on human muscle cells and astrocyte cells. However, the study recognizes the complexity of PARP14, which contains additional macrodomains that might include non-identified epitopes, warranting further investigation.
In conclusion, this research sheds light on a previously overlooked aspect of the immune response against SARS-CoV-2, emphasizing the need for a nuanced understanding of antibody interactions with non-capsid proteins. The implications for COVID-19 patients and the potential risks associated with inactivated viral vaccines call for continued research to refine vaccine strategies and enhance safety protocols. As we navigate the complex landscape of COVID-19, a comprehensive approach to vaccine development and understanding immune responses remains paramount.
The study findings were published in the peer reviewed journal: Vaccines.
https://www.sciencedirect.com/science/article/abs/pii/S0264410X24000999
For the latest
COVID-19 News, keep on logging to Thailand Medical News.