Nikhil Prasad Fact checked by:Thailand Medical News Team Jun 12, 2024 1 year, 6 months, 1 week, 4 days, 13 hours, 52 minutes ago
Cancer News: Colorectal cancer (CRC) ranks among the most prevalent malignancies worldwide, posing a significant threat to public health. In Western countries, it is the second leading cause of cancer-related deaths. In China, the scenario is similarly alarming, with CRC being the third leading cause of cancer mortality. Typically, the risk of CRC escalates with age, and recent statistics indicate a growing number of cases in individuals under 65 years of age. While early-stage CRC patients undergoing surgical treatment can achieve survival rates exceeding 90%, advanced-stage diagnoses remain prevalent, with a survival rate of less than 20% for metastatic CRC.
 Apolipoprotein A-I as a Key Marker in Colorectal Cancer Prognosis
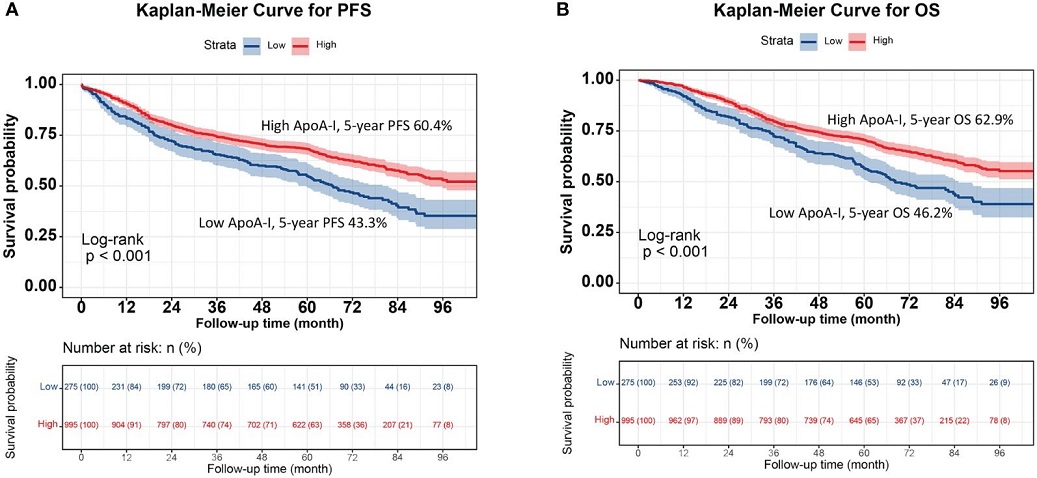
Kaplan-Meier curve of ApoA-I for PFS and OS in patients with colorectal cancer. (A), Kaplan-Meier curve for PFS (High ApoA-I vs Low ApoA-I; 60.4% vs 43.3%); (B), Kaplan-Meier curve for OS (High ApoA-I vs Low ApoA-I; 62.9% vs 46.2%).
Apolipoprotein A-I as a Key Marker in Colorectal Cancer Prognosis
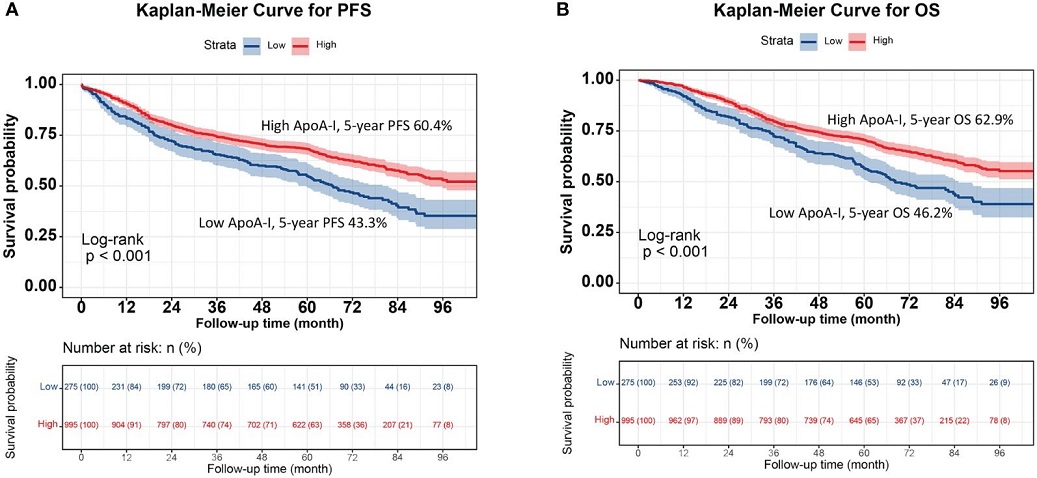
Kaplan-Meier curve of ApoA-I for PFS and OS in patients with colorectal cancer. (A), Kaplan-Meier curve for PFS (High ApoA-I vs Low ApoA-I; 60.4% vs 43.3%); (B), Kaplan-Meier curve for OS (High ApoA-I vs Low ApoA-I; 62.9% vs 46.2%).
The Significance of Apolipoprotein A-I
The role of lipids in cancer progression has gained considerable attention. Apolipoprotein A-I (ApoA-I), a key component of high-density lipoproteins (HDL), is primarily synthesized in the liver and is known for its cholesterol transport, antioxidant properties, anti-inflammatory effects, and anticoagulant activities.
Previous studies have indicated its protective role against cardiovascular diseases. However, its relationship with various cancers, including renal cell carcinoma, esophageal squamous cell carcinoma, nasopharyngeal carcinoma, ovarian cancer, non-small cell lung cancer, and bladder cancer, has been explored with mixed outcomes.
The Study's Objective and Methods
The study covered in this
Cancer News report aimed to investigate the significance of ApoA-I levels in the progression-free survival (PFS) and overall survival (OS) of CRC patients.
Conducted at the First Affiliated Hospital of Guangxi Medical University-China, the study included 1,270 CRC patients treated between 2015 and 2017. Participants were selected based on criteria such as no preoperative treatments, postoperative pathological confirmation of CRC, availability of complete clinical and pathological data, and being aged 18 years or older.
Data collection encompassed various clinical parameters, including age, sex, body mass index (BMI), medical history, serum lipid parameters, and postoperative examination reports. The follow-up period ranged from one month to 106 months, with a median of 64.9 months. Statistical analyses included Kaplan-Meier survival curves, Cox proportional hazards regression models, and logistic regression analysis to explore the relationship between ApoA-I levels and disease outcomes.
Key Findings
The study's results were illuminating. Patients were divided into low (<0.9 g/L) and high (≥0.9 g/L) ApoA-I groups. The h
igh ApoA-I group demonstrated significantly higher survival rates compared to the low ApoA-I group, with PFS rates of 64.8% versus 45.2% and OS rates of 66.1% versus 48.6%. Each one-standard-deviation increase in ApoA-I levels was associated with a 12.0% decrease in PFS risk and an 11.2% decrease in OS risk. Additionally, patients with low ApoA-I had a 32.5% increased risk of disease recurrence compared to those with high ApoA-I levels.
Comparative Analysis of Lipid Indicators
Among various lipid indicators, ApoA-I showed superior predictive accuracy for CRC prognosis. The study highlighted that high ApoA-I levels correlated with better survival outcomes and lower risks of disease recurrence. This finding was consistent across different subgroups, including those categorized by TNM stage, tumor location, and carcinoembryonic antigen (CEA) levels.
Developing Prognostic Nomograms
The study further developed PFS and OS nomograms based on ApoA-I levels, age, TNM stage, and CEA levels. These nomograms demonstrated high predictive performance, with the C-index for OS and PFS being 0.726 and 0.719, respectively. The inclusion of ApoA-I in prognostic models provided a more accurate prediction of patient outcomes compared to traditional TNM staging alone.
Implications for Clinical Practice
The findings underscore the potential of serum ApoA-I levels as a valuable, non-invasive biomarker for predicting CRC patient outcomes. Low ApoA-I levels were significantly associated with advanced pathological staging, larger tumor diameters, and higher CEA levels. Therefore, monitoring ApoA-I levels could help clinicians identify patients at higher risk of poor outcomes and tailor treatment strategies accordingly.
Limitations and Future Research
Despite its strengths, the study had some limitations. The retrospective single-center design might have introduced selection bias, and the study population consisted solely of Chinese individuals. Further research is necessary to validate these findings in diverse populations and explore the applicability of ApoA-I-based prognostic models in clinical settings.
Conclusion
This study adds to the growing body of evidence supporting the role of lipid metabolism in cancer prognosis. Serum ApoA-I levels emerged as a significant prognostic marker in CRC, offering insights that could enhance patient care and treatment planning. By integrating ApoA-I levels with traditional prognostic tools, clinicians can achieve a more comprehensive assessment of CRC outcomes, ultimately improving patient management and survival rates.
The study findings were published in the peer reviewed journal: Frontiers in Endocrinology.
https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1318416/full
For the latest
Cancer News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/new-hope-for-colorectal-cancer-treatment-traditional-chinese-medicine-takes-the-spotlight
https://www.thailandmedical.news/news/metformin-targets-colorectal-cancer-cell-growth-via-mirna-regulation
https://www.thailandmedical.news/news/removal-of-appendix-associated-with-lower-risk-of-developing-certain-types-of-colorectal-cancers