Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 23, 2025 3 weeks, 2 days, 5 hours, 16 minutes ago
Medical News: A New Key Player in Autoimmune Disease Mechanisms
In a groundbreaking discovery that could revolutionize the way autoimmune diseases are understood and treated, scientists from the University of Pennsylvania’s Perelman School of Medicine, Washington University School of Medicine in St Louis, and the Sanford Burnham Prebys Medical Discovery Institute in the United States have uncovered the critical role of a little-known protein called ArfGAP2. This protein has now been identified as a major contributor to harmful immune overreactions that cause damage in autoimmune diseases, opening the door to promising new treatment strategies.
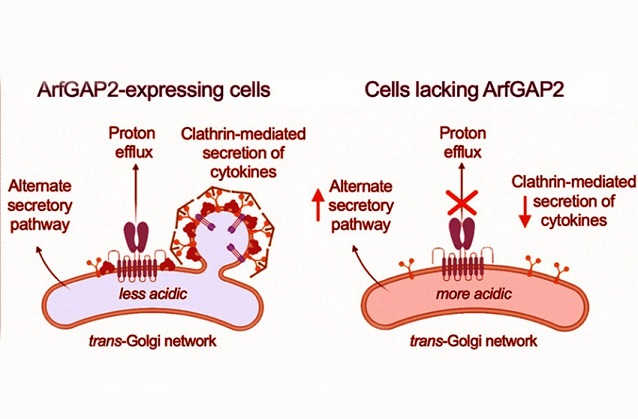
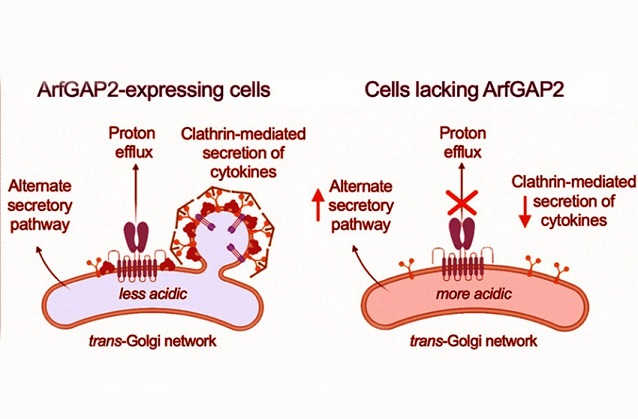 Graphical Abstract:ArfGAP2 Identified as a Hidden Driver of Autoimmune Disorders
Graphical Abstract:ArfGAP2 Identified as a Hidden Driver of Autoimmune Disorders
Autoimmune disorders, which affect over 15 million people in the United States alone, occur when the body’s own immune system mistakenly attacks healthy tissues, believing them to be foreign threats. These misguided attacks lead to chronic inflammation, pain, and damage to organs such as the lungs, brain, skin, and joints. While much research has focused on what triggers the immune system to go rogue, the exact mechanisms behind the immune system’s full-scale attack responses have remained largely elusive - until now.
In this
Medical News report, we delve into how this breakthrough was made possible through the study of an ultra-rare and deadly condition known as STING-associated vasculopathy with onset in infancy (SAVI), and how researchers uncovered the pivotal role of ArfGAP2 in the body's inflammatory processes. The findings not only shed light on the inner workings of autoimmune disease but may also lead to better treatments for conditions such as lupus, multiple sclerosis, rheumatoid arthritis, COVID-19-related cytokine storms and autoimmune issues, and even neurodegenerative diseases like Alzheimer’s.
How a Rare Disease Helped Unlock a Widespread Medical Mystery
The new study was co-led by Dr. Jonathan Miner, MD, PhD, an associate professor of Rheumatology and Microbiology and a member of Penn’s Colton Center for Autoimmunity, and Dr. David Kast, PhD, an assistant professor in the Department of Cell Biology and Physiology at Washington University School of Medicine.
Their research focused on SAVI, a rare genetic disease that affects only one in every million births. SAVI causes the body’s immune system to relentlessly attack its own tissues, especially the lungs and limbs. Tragically, many patients with SAVI do not survive past childhood due to the severe internal damage caused by their overactive immune systems.
SAVI is caused by mutations in a protein called STING (Stimulator of Interferon Genes), which normally acts as a sensor that detects viral DNA inside cells and triggers the production of cytokines - immune signaling molecules that help coordinate the body’s defenses. However, in SAVI patients, the STING protein is stuck in the “on” position, sending constant immune alerts even when no infection is present. This causes a continuous release of inflammatory molecules that damage tissues
throughout the body.
From Signal to Secretion: The Crucial Role of ArfGAP2
While scientists have long known that STING signals the body to produce cytokines, what remained unclear was how these cytokines were actually transported out of cells to trigger the immune response. That’s where ArfGAP2 comes in.
Using genetically engineered immune cells that mimicked the conditions seen in SAVI, the researchers screened for proteins that might be involved in this final step of immune signaling - the release of cytokines from the cell. Among hundreds of proteins examined, one stood out: ArfGAP2.
Further experiments confirmed that ArfGAP2 acts like a cellular traffic controller. When ArfGAP2 was missing, STING could still signal for cytokine production inside the cell - but the cytokines couldn’t get out. This meant that although the immune system was still being “alerted,” it couldn’t mount its destructive attack without ArfGAP2 helping to release the cytokines into the body.
“It’s like a train station where ArfGAP2 is the conductor,” explained Dr. Kast. “Without it, the immune molecules just pile up inside the cell with nowhere to go. They can’t trigger an inflammatory response without ArfGAP2 directing the traffic.”
Turning Off the Damage in Animal Models
To see if this discovery could have real-world therapeutic implications, the team created a mouse model of SAVI in which the mice lacked ArfGAP2. Incredibly, the immune system’s attack on the lungs and limbs - which usually devastates the mice - was almost completely stopped. Without ArfGAP2, the overactive STING protein was no longer able to drive the release of inflammatory cytokines, effectively silencing the self-destructive immune response.
This finding is particularly exciting because it proves that ArfGAP2 is not just a participant in the disease process - it’s essential to it. Blocking or deleting ArfGAP2 halted the progression of the autoimmune damage, suggesting that new drugs designed to target this protein could offer a powerful and focused way to treat autoimmune conditions.
Broader Implications for Other Diseases
Even more exciting is the possibility that ArfGAP2 may play a role in many other immune-related conditions beyond SAVI. Dr. Miner emphasized that the type of inflammatory cytokines regulated by STING and ArfGAP2 are also involved in the “cytokine storms” that make COVID-19 so deadly and are increasingly being implicated in Alzheimer’s disease, where the brain's immune responses spiral out of control.
“By studying an ultra-rare disease like SAVI, we’ve uncovered a completely new way the immune system is regulated,” said Dr. Miner. “This helps us understand not only rare diseases but also common and devastating conditions. The same proteins that go haywire in SAVI are present in all of us, and if we can control them, we can potentially control a wide range of inflammatory diseases.”
Digging Deeper into the Science
The research also revealed a novel function of the STING protein - acting as a proton channel that controls the acidity of a cell structure called the Golgi apparatus, which is responsible for packaging and shipping proteins like cytokines. ArfGAP2 was shown to be essential in this process, facilitating proton efflux from the Golgi and ensuring proper cytokine trafficking.
When ArfGAP2 was deleted specifically in blood-forming (hematopoietic) and blood vessel (endothelial) cells in mice, researchers observed a marked reduction in STING-mediated inflammation, immune cell activation, and cytokine secretion. These detailed findings further highlight how critical ArfGAP2 is to the final step of the immune signaling process and its potential as a target for drug development.
A Hopeful Outlook for Future Treatments
The conclusions drawn from this study are profound. First, it demonstrates the incredible potential of rare disease research to inform broader medical science. Second, it identifies a precise, druggable target- ArfGAP2 - that could potentially be modulated to treat a wide range of immune-related diseases. Most importantly, it shows that the immune system’s destructive responses can be dialed down without completely shutting it off, offering a more refined way to manage autoimmune diseases without suppressing the immune system entirely.
Future therapies based on ArfGAP2 inhibition could revolutionize how we treat chronic inflammation, allowing physicians to calm the immune system only when necessary, and only in the tissues being damaged - minimizing side effects while maximizing effectiveness. This new line of research may soon lead to the development of first-in-class drugs that could help millions suffering from autoimmune diseases, infectious complications like cytokine storms, and neuroinflammatory disorders. With further studies and clinical trials, ArfGAP2 inhibitors may become a new cornerstone of precision medicine in immunology.
The study findings were published in the peer reviewed journal: Cell.
https://www.cell.com/cell/abstract/S0092-8674(25)00096-0
For the latest COVID-19 News, keep on logging to Thailand
Medical News
Read Also:
https://www.thailandmedical.news/news/list-of-86-of-167-autoantibodies-that-covid-19-infections-and-vaccines-induces-in-the-human-host-part1
https://www.thailandmedical.news/news/scientists-discover-a-highly-conserved-region-in-the-sars-cov-2-spike-protein-that-triggers-harmful-autoantibodies
https://www.thailandmedical.news/news/it-was-wrong-to-have-used-the-spike-proteins-in-the-covid-19-vaccines-as-they-can-elicit-many-kinds-of-pathogenic-autoantibodies
https://www.thailandmedical.news/pages/thailand_doctors_listings
Follow us on:
https://x.com/ThailandMedicaX
https://www.facebook.com/ThailandMedicalNews
https://bsky.app/profile/thailandmedical.bsky.social
https://gettr.com/user/thailandmedicalnews
https://www.tribel.com/thailandmedical/wall
and 33 other social media platforms