Assessing Peripheral and Organ Perfusion to Identify High-Risk COVID-19 Patients
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 12, 2024 1 year, 1 month, 3 weeks, 4 days, 16 hours, 3 minutes ago
Medical News: The COVID-19 pandemic brought unprecedented challenges to healthcare systems worldwide, with severe cases often resulting in life-threatening complications such as organ failure and respiratory distress. Researchers from the Military Institute of Medicine-National Research Institute in Warsaw, Poland, conducted a groundbreaking study to assess the role of peripheral and organ perfusion in predicting disease severity and mortality among severe COVID-19 patients. This
Medical News report delves into the study’s findings, which underscore the critical importance of monitoring perfusion parameters to identify high-risk patients early.
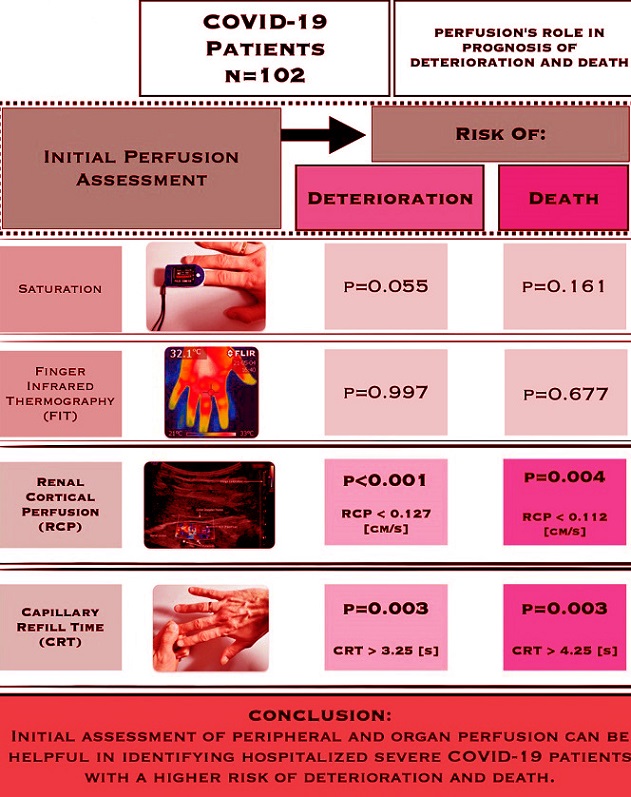
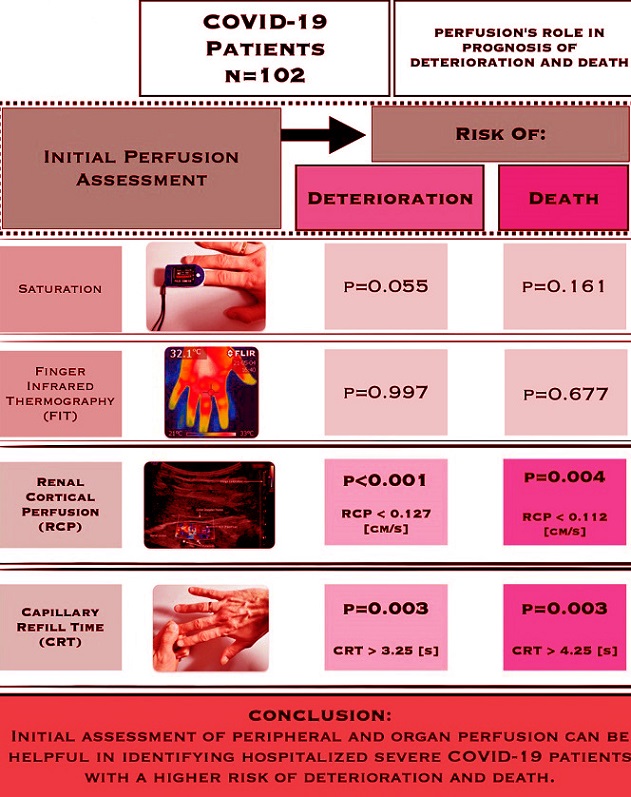 Graphical Abstract - Assessing Peripheral and Organ Perfusion to Identify High-Risk COVID-19 Patients
Understanding Perfusion and Its Role in COVID-19
Graphical Abstract - Assessing Peripheral and Organ Perfusion to Identify High-Risk COVID-19 Patients
Understanding Perfusion and Its Role in COVID-19
Perfusion refers to the flow of blood through the body’s tissues and organs, ensuring they receive adequate oxygen and nutrients. In severe COVID-19 cases, the virus triggers a systemic inflammatory response, leading to microcirculation disorders. These disruptions often culminate in organ dysfunction and increased mortality. The study highlights how assessing specific perfusion markers can offer valuable insights into a patient’s prognosis.
One of the key challenges in managing COVID-19 has been distinguishing patients likely to deteriorate from those with a stable course. By evaluating peripheral perfusion markers such as Capillary Refill Time (CRT) and Finger Infrared Thermography (FIT), along with organ perfusion metrics like Renal Cortical Perfusion (RCP), the study aimed to address this critical gap.
Study Design and Methodology
The study was conducted during the COVID-19 pandemic at the Temporary Hospital of the Military Institute of Medicine in Warsaw. It involved 102 patients diagnosed with severe COVID-19 and requiring oxygen therapy. Patients were closely monitored within the first 48 hours of hospitalization to assess their perfusion parameters.
Researchers used various non-invasive methods, including:
-Capillary Refill Time (CRT): Measuring the time it takes for color to return to the skin after pressure is applied.
-Finger Infrared Thermography (FIT): Capturing thermal images of the fingers to analyze blood flow.
-Renal Cortical Perfusion (RCP): Utilizing Doppler ultrasound to measure blood flow in the kidney’s cortex.
Additional metrics, such as blood oxygen levels and laboratory markers of inflammation, were also recorded. These measurements provided a comprehensive overview of the patients’ physiological status.
Key Findings
The study revealed significant associations between perfusion parameters and patient outcomes. Out of the 102 patients, 40 experienced a worsening of symptoms, requiring advanced oxygen therapy, and 24 succumbed to the disease.<
;br />
The findings highlighted two critical markers:
-Capillary Refill Time (CRT): Patients with prolonged CRT were more likely to experience deterioration or death. Specifically, a CRT value exceeding 3.25 seconds indicated a heightened risk of clinical worsening, while values above 4.25 seconds were associated with increased mortality. CRT emerged as a reliable indicator of peripheral perfusion, reflecting systemic blood flow inadequacies.
-Renal Cortical Perfusion (RCP): Lower RCP values correlated strongly with poorer outcomes. The study identified an RCP threshold of 0.127 cm/s for predicting deterioration and 0.112 cm/s for mortality. Reduced RCP suggests compromised kidney perfusion, a hallmark of severe illness.
Interestingly, other parameters such as FIT and oxygen saturation were not statistically significant predictors of outcomes. While FIT provided useful supplementary data, it lacked the predictive power of CRT and RCP.
The Implications for Clinical Practice
The findings have profound implications for the management of severe COVID-19 cases. By incorporating CRT and RCP assessments into routine clinical evaluations, healthcare providers can:
-Early Identification: Detect high-risk patients earlier, allowing for timely interventions.
-Tailored Treatments: Allocate resources more effectively, focusing intensive care on those most likely to benefit.
-Improved Prognostication: Enhance communication with families about potential outcomes based on objective metrics.
Moreover, these assessments are non-invasive, cost-effective, and easily implementable in resource-limited settings, making them valuable tools in global healthcare.
Limitations and Future Directions
While the study provides valuable insights, it also highlights some limitations. For instance, CRT and ultrasound measurements are operator-dependent, requiring standardized training to ensure accuracy. Additionally, the study focused exclusively on COVID-19 patients, so the findings may not generalize to other diseases.
Future research should explore the applicability of these perfusion markers in other critical illnesses, such as sepsis and acute respiratory distress syndrome (ARDS). Expanding the study population and incorporating automated measurement technologies could further enhance reliability and scalability.
Conclusions
This study underscores the pivotal role of peripheral and organ perfusion assessments in managing severe COVID-19. Capillary Refill Time and Renal Cortical Perfusion emerged as robust predictors of deterioration and mortality, offering a lifeline for early intervention. These findings pave the way for more personalized and effective care strategies, ultimately improving patient outcomes.
The study findings were published in the peer-reviewed Journal of Clinical Medicine.
https://www.mdpi.com/2077-0383/13/24/7520
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-alters-brain-blood-flow
https://www.thailandmedical.news/news/covid-19-causes-morphological-changes-of-red-blood-cells-leading-to-microangiopathy-microthrombosis-impaired-blood-flow-tissue-oxygenation
https://www.thailandmedical.news/articles/coronavirus