Association Between Lipid Levels, Anti-SARS-CoV-2 Spike Antibodies, And COVID-19 Mortality - New Research Unravels The Immune Puzzle
Thailand Medical News Team Aug 07, 2023 1 year, 7 months, 3 weeks, 21 hours, 39 minutes ago
COVID-19 Research: The COVID-19 pandemic has challenged the global healthcare system, leading scientists and researchers to explore various factors that influence disease outcome. A recent study conducted by Central Medical Laboratories in Austria, the Private University of the Principality of Liechtenstein, the Academic Teaching Hospital Feldkirch in Austria, and Drexel University College of Medicine in the USA has shed light on a compelling association between lipid levels, anti-SARS-CoV-2 spike antibodies, and COVID-19 mortality.
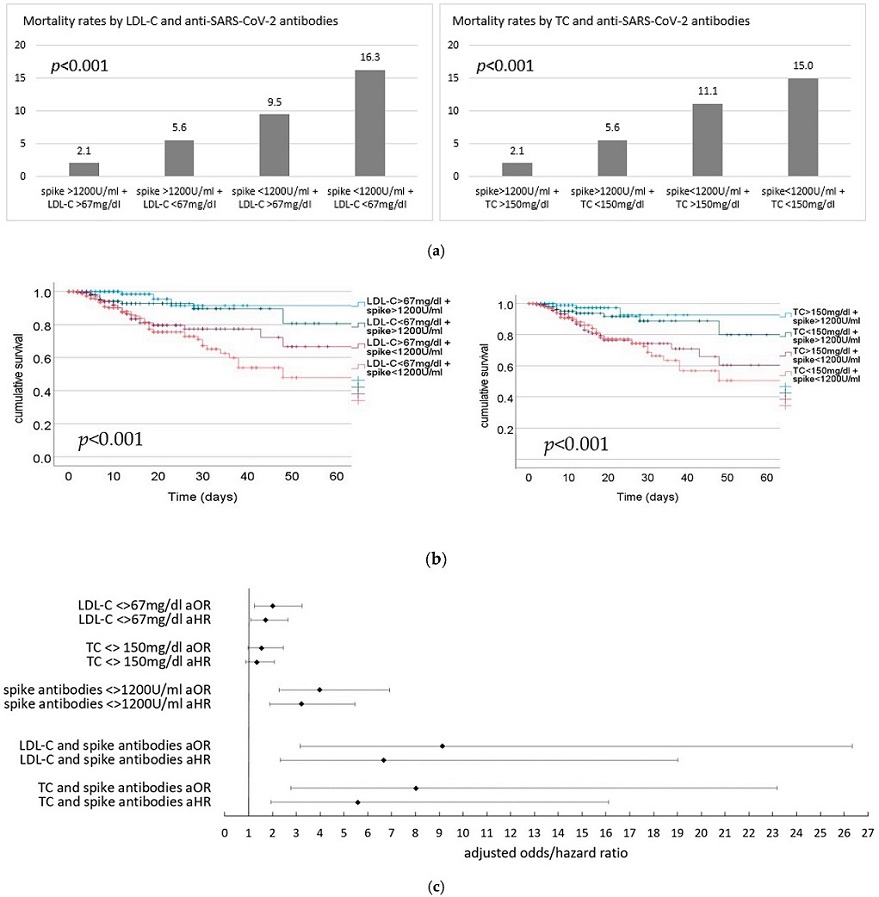
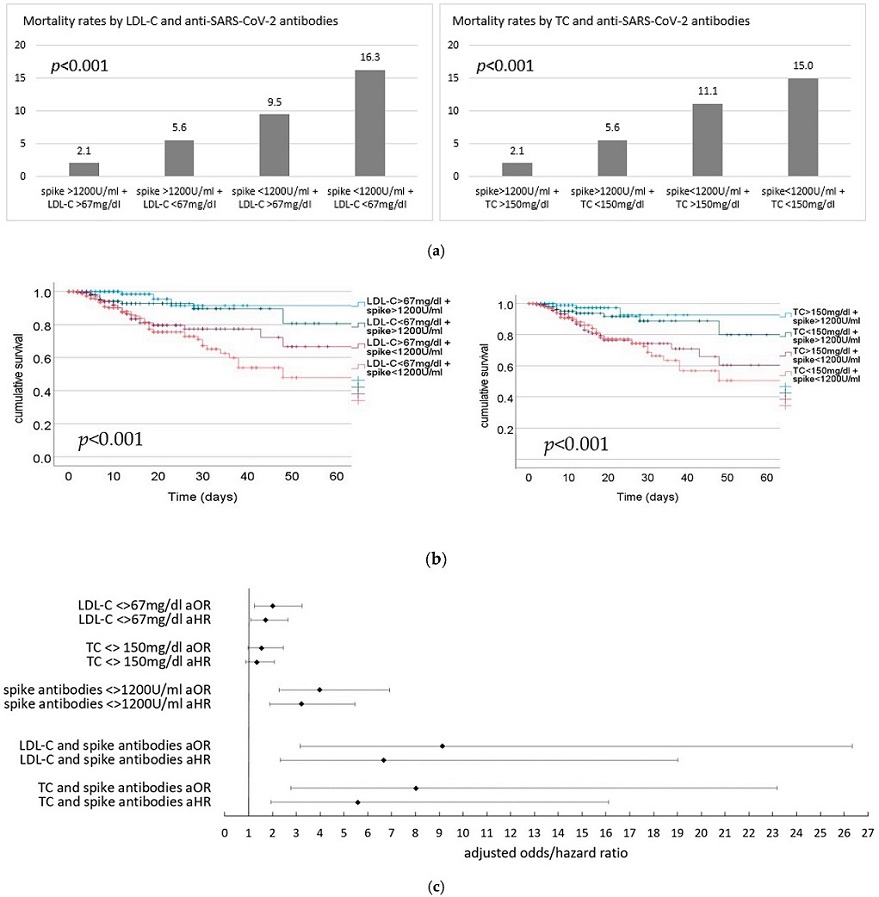 (a) Mortality rates (%) by LDL-C (left)/TC (right) and anti-SARS-CoV2-spike antibodies. TC total cholesterol. (b) Cumulative survival over time in days depending on lipid and anti-SARS-CoV2 spike antibody levels; LDL-C (left) and TC (right). TC total cholesterol. (c) Adjusted odds and hazard ratios for in-hospital mortality for lipid levels (below vs. above the respective median value), anti SARS-CoV2 antibodies (<>1200 U/mL) as well as aOR/aHR for low vs. high levels of both lipid level and anti-SARS-CoV2 spike antibodies. TC total choles-terol, spike antibodies—anti-SARS-CoV2-spike antibodies.
(a) Mortality rates (%) by LDL-C (left)/TC (right) and anti-SARS-CoV2-spike antibodies. TC total cholesterol. (b) Cumulative survival over time in days depending on lipid and anti-SARS-CoV2 spike antibody levels; LDL-C (left) and TC (right). TC total cholesterol. (c) Adjusted odds and hazard ratios for in-hospital mortality for lipid levels (below vs. above the respective median value), anti SARS-CoV2 antibodies (<>1200 U/mL) as well as aOR/aHR for low vs. high levels of both lipid level and anti-SARS-CoV2 spike antibodies. TC total choles-terol, spike antibodies—anti-SARS-CoV2-spike antibodies.
Previous
COVID-19 Research has hinted at the role of plasma lipoproteins in eliminating pathogen-associated lipids and toxins during severe infections like sepsis. However, their exact significance in COVID-19 remains unclear.
Similarly, anti-SARS-CoV-2 spike antibodies have been linked to lower infection rates and protection against severe COVID-19 courses. Positive outcomes were observed following the administration of neutralizing monoclonal antibodies and booster vaccinations.
Given these clues, the study team sought to explore the relationship between lipoproteins, antibodies, and COVID-19 mortality.
In a prospective, multicenter cohort study, 1152 hospitalized patients with COVID-19 were recruited from five hospitals. The study team measured total cholesterol (TC), LDL cholesterol (LDL-C), HDL cholesterol (HDL-C), triglycerides, and anti-SARS-CoV-2 spike antibodies on admission, and the endpoint of interest was in-hospital mortality.
The study findings revealed a significant association between lipid levels and COVID-19 mortality. Non-survivors had considerably lower LDL-C, HDL-C, and TC levels compared to survivors. The risk of mortality increased progressively with decreasing levels of these lipids.
Strikingly, mortality rates varied drastically based on the combination of LDL-C or TC levels and anti-SARS-CoV-2 spike antibodies. Patients with high levels of both LDL-C or TC and antibodies had the lowest mortality rates, while those with low levels of both parameters had the highest mortality rates.
These study findings support previous research indicating an association between lipid levels and COVID-19 mortality. Patients with severe COVID-19 often exhibit lower total cholesterol, HDL-C, and LDL-C levels. However, triglyceride levels did not show significant differences in outcome in this study, suggesting that their role in COVID-19 severity may vary from that of other lipids.
The exact pathophysiological role of lipoproteins in COVID-19 is not fully understood, but they are believed to play a crucial role in the removal of pathogen-associated lipids and toxins. Lower lipid levels in COVID-19 patients could indicate an impairment of this vital process, while higher lipid levels may reflect a better general condition of the individual. Additionally, the function of lipoproteins may also be impaired in severe COVID-19 cases, further contributing to the disease severity.
On the other hand, antibodies are known to be vital in neutralizing pathogens. Previous studies have demonstrated that neutralizing antibodies are correlated with protection against severe COVID-19. The administration of neutralizing monoclonal antibodies and booster vaccinations has shown positive effects in the prevention and treatment of COVID-19. Furthermore, higher anti-SARS-CoV-2 spike antibody levels upon hospital admission have been associated with lower in-hospital mortality.
Hypothetically, lipoproteins could be involved in the removal of previously neutralized SARS-CoV-2 particles by antibodies. However, whether the association between lipoprotein and antibody levels and COVID-19 mortality indicates a pathophysiological mechanism or simply reflects a better general condition of the patients requires further investigation.
This study's strengths lie in its high recruitment rate and the use of in-hospital mortality as a robust endpoint. Multiple potential confounders were adjusted for, including statin therapy and known risk factors for severe COVID-19.
Nevertheless, additional studies are needed to determine protective cutoff levels of lipoproteins and antibodies against negative COVID-19 outcomes. The findings hint at a potential synergistic pathophysiological mechanism involving both lipoproteins and antibodies, but further research is required to confirm this relationship and understand the precise underlying mechanisms.
Understanding the combined role of lipoproteins and antibodies in severe infections like COVID-19 could identify high-risk patients and enable timely adjustments to therapy. Moreover, it may offer new avenues for future pharmacological therapeutic approaches. This study underscores the complexity of the immune response against SARS-CoV-2 and opens up new avenues for exploring personalized approaches to COVID-19 treatment and management.
In conclusion, this groundbreaking research demonstrates that LDL-C and TC levels, in conjunction with anti-SARS-CoV-2 spike antibodies, strongly predict in-hospital mortality in COVID-19 patients. The study emphasizes the importance of considering both lipoproteins and antibodies as critical players in the immune response against SARS-CoV-2.
The study findings were published in the peer reviewed Journal of Clinical Medicine.
https://www.mdpi.com/2077-0383/12/15/5068
For the latest
COVID-19 Research, keep on logging to Thailand Medical News.