BREAKING! Australian Scientists Uncover a New Approach That Might End Autoimmune Diseases for Good!
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 24, 2025 3 weeks, 3 days, 19 hours, 8 minutes ago
Medical News: A groundbreaking study by Australian researchers from the Garvan Institute of Medical Research, the University of New South Wales, and St Vincent’s Hospital Sydney is shaking up the world of autoimmune disease treatment. Dr. Dan Suan, Dr. John Moore, and Professor Christopher C. Goodnow have revealed that a deeper, more targeted immune therapy could do more than just relieve symptoms - it might actually cure these diseases.
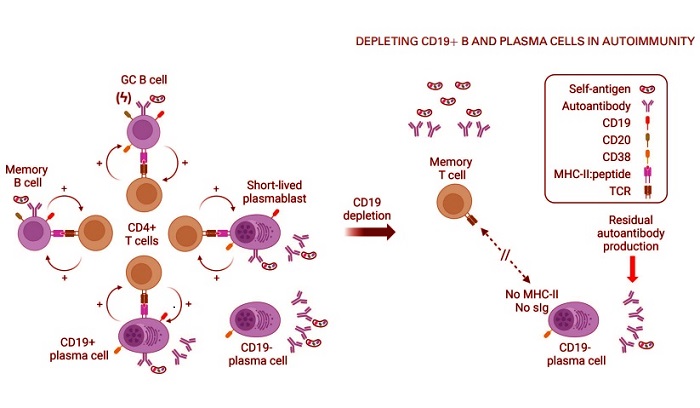
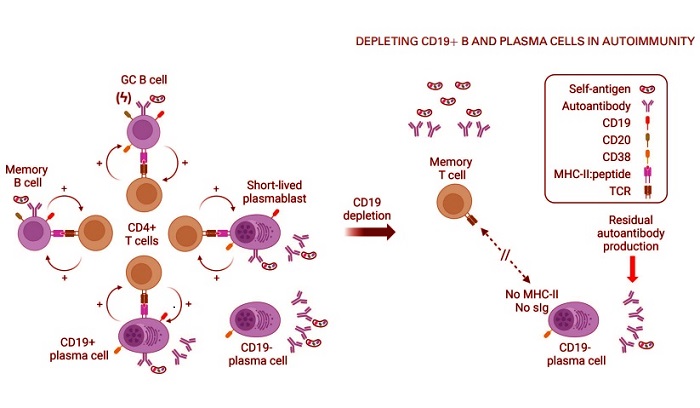 Autoimmune disease is driven by autoantibody-bearing CD19þ plasma cells and B cells perpetuating cellular responses to self-antigens that are never cleared but are abolished by deep CD19 compartmental depletion. In autoimmune disease (left), clonal proliferation and increased affinity of self-reactive surface Ig in germinal center (GC) or extrafollicular reactions (ϟ) creates a high frequency of CD19þ cells using the PAX5 B cell gene expression program to stimulate CD4þ T cells, which in turn stimulate the CD19þ plasma cells and B cells. The process is self-perpetuating (þ) and enlists more B and T cell clones because the self-antigen is not cleared. After deep CD19þ cell depletion (right), all B cells and CD19þ plasma cell clones with the capacity to ingest self-antigen and present peptide to T cells are eradicated, leading to resolution of the cellular reaction despite the persistent presence of self-antigen, with T cells returning to a quiescent memory T cell state. Residual CD19 - plasma cells that are not deleted by anti-CD19 therapies, if they exist in the individual, continue to produce a stable quantum of autoantibody (red arrow), but these cells possess no ability to communicate with T cells due to the absence of surface autoantibody or MHC-II, and a small quantum of autoantibody alone does not sustain a self-perpetuating autoimmune response, permitting individuals to enter a drug-free, clinical remission.
Autoimmune disease is driven by autoantibody-bearing CD19þ plasma cells and B cells perpetuating cellular responses to self-antigens that are never cleared but are abolished by deep CD19 compartmental depletion. In autoimmune disease (left), clonal proliferation and increased affinity of self-reactive surface Ig in germinal center (GC) or extrafollicular reactions (ϟ) creates a high frequency of CD19þ cells using the PAX5 B cell gene expression program to stimulate CD4þ T cells, which in turn stimulate the CD19þ plasma cells and B cells. The process is self-perpetuating (þ) and enlists more B and T cell clones because the self-antigen is not cleared. After deep CD19þ cell depletion (right), all B cells and CD19þ plasma cell clones with the capacity to ingest self-antigen and present peptide to T cells are eradicated, leading to resolution of the cellular reaction despite the persistent presence of self-antigen, with T cells returning to a quiescent memory T cell state. Residual CD19 - plasma cells that are not deleted by anti-CD19 therapies, if they exist in the individual, continue to produce a stable quantum of autoantibody (red arrow), but these cells possess no ability to communicate with T cells due to the absence of surface autoantibody or MHC-II, and a small quantum of autoantibody alone does not sustain a self-perpetuating autoimmune response, permitting individuals to enter a drug-free, clinical remission.
For decades, doctors have been fighting autoimmune disorders using drugs like rituximab that target B cells marked by a protein called CD20. These treatments have helped, but they rarely provide lasting remission. Most patients relapse, requiring repeated therapy. Now, thanks to new insights and this
Medical News report, attention is shifting toward a broader but more precise target - CD19 - found on even more B cell types, including a hidden population responsible for stubborn disease relapses.
What is CD19?
CD19 is a protein found on the surface of B cells, a type of white blood cell crucial for the immune system. It acts as a co-receptor for the B-cell antigen receptor complex (BCR), lowering the threshold for B cell activation and enhancing the immune response to antigens. By forming a complex with other proteins like CD21 and CD81, CD19 plays a central role in B cell development, proliferation, and antibody production. Due to its consistent presence on B cells, CD19 serves as a reliable biomarker for diagnosing B cell-related conditions and is a target in therapies for diseases like leukemia and lymphoma.
Why CD19 Is the New Target in Autoimmunity&l
t;br />
Autoimmune diseases, such as lupus, type 1 diabetes, and rheumatoid arthritis, are caused when the body’s immune system mistakenly attacks its own cells. One of the main culprits behind this attack is a group of immune cells called B cells that produce harmful autoantibodies.
Until recently, most treatments have focused on eliminating B cells that express CD20. However, new research shows that many dangerous B cells and plasma cells responsible for autoantibody production do not carry CD20 but still express CD19. These include long-lived, mutated cells that continue to drive the disease even after CD20-targeting drugs like rituximab have done their job.
In two compelling case studies, the researchers showed that patients with severe autoimmune conditions, including cryoglobulinemic vasculitis and cerebellar ataxia, had rogue B cells that expressed CD19 but not CD20. These CD19+ cells survived rituximab therapy and continued producing disease-causing antibodies.
Why Standard Treatments Often Fail
One reason rituximab doesn’t always work is that it can’t reach every part of the body efficiently. In places like the salivary glands or brain tissue, it struggles to eliminate all the CD20+ cells. Worse still, the most harmful clones often lack CD20 entirely, allowing them to slip under the radar and keep causing damage.
These CD19+ plasma cells aren’t just antibody factories—they still carry receptors on their surface and can interact with other immune cells, fueling a vicious cycle of inflammation. Researchers liken these cells to “half-transformed” B cells that haven’t completely let go of their original identity and function, making them uniquely dangerous and hard to treat.
Anti-CD19 CAR T Cell Therapy Produces Stunning Results
One of the most exciting parts of the study comes from the use of anti-CD19 CAR T cell therapy - a type of treatment where a patient’s own immune cells are modified to hunt and destroy CD19+ cells. Originally designed for leukemia and lymphoma, this approach has now been tested in patients with severe autoimmune diseases who failed to respond to standard treatments.
The results were nothing short of miraculous. Patients with lupus, myositis, systemic sclerosis, and other serious conditions went into full remission. Their symptoms vanished, lab tests normalized, and many were able to stop all other medications. Most importantly, they remained disease-free for years.
These early successes suggest that CD19 CAR T cell therapy doesn't just suppress the disease - it might actually erase the immune memory that drives it, something no other therapy has been able to do.
How CD19+ Plasma Cells Keep Autoimmune Diseases Alive
Scientists used to believe that plasma cells - the antibody producers - were terminally differentiated, meaning they were permanently locked into their role. However, this study turns that belief upside down. In humans, most plasma cells continue to express CD19 and other B cell-related genes.
That means these plasma cells can still recognize and present autoantigens to T cells, acting like antigen-presenting cells. This ability helps them maintain the damaging immune response and keeps the autoimmune fire burning. These CD19+ plasma cells are also long-lived. In some cases, they’ve been found to survive in tissues like the bone marrow or intestines for over 20 years.
The researchers also found that these cells are especially common in tissues affected by autoimmune diseases. In celiac disease, for example, CD19+ plasma cells outnumber other immune cells in the gut and present gluten-derived antigens to T cells, keeping the disease active. A similar pattern was seen in rheumatoid arthritis and type 1 diabetes.
Why This Could Be a Turning Point
These findings may finally explain why so many autoimmune diseases are hard to cure. They show that the key driver isn't just the autoantibodies themselves, but the ongoing interaction between CD19+ plasma cells and T cells. This creates a “feedforward loop” that keeps the immune system attacking the body, even if the original trigger is gone.
By targeting CD19, researchers can break this loop - eliminating the dangerous plasma cells and stopping them from talking to T cells. This could be the missing piece in the puzzle of autoimmunity.
Conclusion
This new model challenges decades of thinking about autoimmune disease. It reveals that the hidden population of CD19+ plasma cells play a central role in keeping these diseases alive. Standard therapies have overlooked them, allowing disease to smolder and relapse. Now, with the advent of anti-CD19 therapies - especially CAR T cells - we may have the tools to shut down autoimmune disease at its root. This discovery not only explains past treatment failures but also opens the door to real cures. If larger studies confirm these results, millions of people around the world could one day be free from lifelong autoimmune illness.
The study findings were published in the peer reviewed journal: The Journal of Immunology.
https://academic.oup.com/jimmunol/advance-article/doi/10.1093/jimmun/vkaf008/8090055
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/sars-cov-2-induced-igg-autoantibodies-are-targeting-various-immune-cells-and-also-proteins-in-various-organs
https://www.thailandmedical.news/news/arfgap2-identified-as-a-hidden-driver-of-autoimmune-disorders
https://www.thailandmedical.news/news/covid-19-induced-anti-ganglioside-autoantibodies-is-causing-neuropathy-in-many
https://www.thailandmedical.news/news/list-of-86-of-167-autoantibodies-that-covid-19-infections-and-vaccines-induces-in-the-human-host-part1
https://www.thailandmedical.news/pages/thailand_doctors_listings