BREAKING! British Study Shows That 59 Percent Of Post-COVID Individuals Are Inflicted With Organ Impairment!
Source: Medical News - Organ Impairment In Post-COVID Mar 22, 2022 3 years, 9 months, 1 week, 3 days, 2 hours, 34 minutes ago
British researchers from a leading biotech company in Oxford called Perspectum along with scientist and medical professionals from University of Liverpool, Hull and East Yorkshire Hospitals NHS Foundation Trust, University of Hull, Oxford University Hospitals NHS Foundation Trust, University College London Hospitals NHS Foundation Trust, University College London and Barts Health NHS Trust have in a new long COVID study found that 59% Of Post-COVID individuals are inflicted with organ impairment that affects their quality of life!
This is great news as along with another 138 other studies that Thailand
Medical News has based our hypothesis on, it adds to support this prediction of ours that a majority of people who have been exposed to the SARS-CoV-2 virus or its proteins through infections or whatever other means, irrespective if they were asymptomatic or were only mild symptomatic, will have shortened life spans and might not even make it past another 5 to 8 years though with even newer emerging data, we know think that it will be even shorter and earlier that many of these individuals will eventually suffer health deterioration and succumb to fatal outcomes.
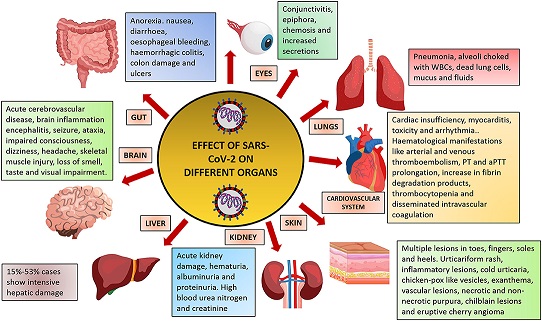
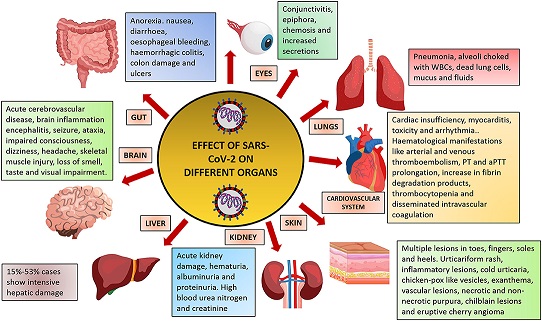
Multi-organ impairment associated with Long COVID is a significant burden to individuals, populations and health systems, presenting challenges for diagnosis and care provision.
To date, standardized assessment across multiple organs over time is lacking, particularly in non-hospitalized individuals.
The study team aim was to determine the prevalence of organ impairment in Long COVID patients at 6 and at 12 months after initial symptoms and to explore links to clinical presentation.
The research involved a prospective, longitudinal study in individuals following recovery from COVID-19.
The study team assessed symptoms, health status, and multi-organ tissue characterization and function, using consensus definitions for single and multi-organ impairment.
Detailed physiological and biochemical investigations were performed at baseline on all individuals and those with organ impairment were reassessed, including multi-organ MRI, 6 months later.
The study involved two non-acute settings at Oxford and London.
https://clinicaltrials.gov/ct2/show/NCT04369807
The study involved 536 individuals (mean 45 years, 73% female, 89% white, 32% healthcare workers who had completed baseline assessment (median: 6 months post-COVID-19).
A total of 331 (62%) with organ impairment or incidental findings had follow up, with reduced symptom burden from baseline (median number of symptoms: 10 and 3, at 6 and 12 months).
All participants had a SARS-CoV-2 infection 6 months prior to first assessment.
The study findings uncovered the following conditions among the participants: Extreme breathlessness (36% and 30%), cognitive dysfunction (50% and 38%) and poor health-related quality of life (EQ-5D-5L<0.7; 55% and 45%) were common at 6 and 12 months, and associated with female gender, younger age and single organ impairment.
Importantly, at baseline, there was fibro-inflammation in the heart (9%), pa
ncreas (9%), kidney (15%) and liver (11%); increased volume in liver (7%), spleen (8%) and kidney (9%); decreased capacity in lungs (2%); and excessive fat deposition in the liver (25%) and pancreas (15%).
Shockingly, single and multi-organ impairment were present in 59% and 23% at baseline, persisting in 59% and 27% at follow-up.
The study findings showed that organ impairment was present in 59% of individuals at 6 months post-COVID-19, persisting in 59% of those followed up at 1 year, with implications for symptoms, quality of life and longer-term health, signaling need for prevention and integrated care of Long COVID.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.medrxiv.org/content/10.1101/2022.03.18.22272607v1
Already previous preliminary MRI data in 201 individuals showed mild organ impairment in the heart, lungs, kidneys, liver, pancreas, and spleen, with single and multi-organ impairment in 70% and 29%, respectively, 4 months after COVID-19. Clinical utility of these MR metrics for chronic and multi-system conditions has been shown. More severe ongoing symptoms of breathlessness and fatigue were associated with myocarditis s (p<0.05)10, but symptoms and multi-organ manifestations have not been correlated.
https://www.frontiersin.org/articles/10.3389/fcvm.2022.854750/abstract
https://pubmed.ncbi.nlm.nih.gov/28520813/
The study findings showed that most standard-of-care biochemical investigations were within normal range and not predictive of outcomes, except lactate dehydrogenase (80/500 [16%] and 70/319 [22%]), creatinine kinase (40/508 [8%] and 41/323 [13%], p=0.03); cholesterol (236/508 [46%] and 157/326 [48%]); and mean cell hemoglobin concentration (106/508 [21%] and 49/324 [15%]) which were elevated at baseline and follow-up.
On MRI of 536 participants at baseline, 59% and 23% had impairment in ≥1 and ≥2 organs respectively. Organ impairment between visits did not improve significantly, unlike symptoms.
At baseline, lung impairment (lower fractional area change) and impairment in ≥3 organs were associated with high symptom burden. At 12 months, there was reduction in symptom burden, except fatigue, breathlessness and reduced HRQoL (Health-related quality of life) where prevalence was unchanged.
The good news was that healthcare workers were more likely to have liver impairment (p=0.017 at baseline and p=0.044 at follow-up) than the rest of the cohort.
Interestingly, in participants without symptoms at follow-up (n=60), organ impairment was present in 43 (72%) at baseline and 37 (62%) at follow-up.
In symptomatic participants at follow-up (n=264), there were 84 (32%) and 112 (42%) without organ impairment at baseline and follow-up, respectively. Liver steatosis, kidney fibro-inflammation and splenomegaly at baseline were more frequent in all symptom groups. Liver steatosis was associated with systemic symptoms and severe breathlessness.
In all, the study showed four new findings:
-1) The study findings confirmed multi-organ impairment at 6- and 12- months in 59% of individuals with Long COVID, with persistent symptoms and reduced function.
-2) Despite some associations between organ impairment and symptoms, there is currently insufficient evidence for distinct Long COVID subtypes. Blood biomarkers, the current standard of care, showed no relation to clinical presentation.
-3) Symptoms, blood investigations and quantitative, multi-organ MRI did not predict trajectory or recovery.
-4) The study findings demonstrate feasibility of scalable, multi-organ assessment in non-acute settings in the pandemic context.
Already several studies confirm persistence of symptoms in individuals with Long COVID up to 1 year.
https://pubmed.ncbi.nlm.nih.gov/34811387/
https://europepmc.org/article/med/35075531
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8875269/
The study findings now add that 3 in 5 people with Long COVID will have impairment in at least one organ, and 1 in 4 have impairment in two or more organs, in some cases without symptoms.
Importantly, the study team observed associations with markers of liver dysfunction, and increased risk of symptoms in female and obese individuals with Long COVID, which has been shown previously.
https://pubmed.ncbi.nlm.nih.gov/33789877/
https://pubmed.ncbi.nlm.nih.gov/33692530/
Cognitive impairment appears to develop in the natural history of Long COVID in some patients. As it is also associated with liver inflammation, it may be that, as with hepatic encephalopathy, disordered liver metabolism and gluconeogenesis may cause abnormal brain function. However, underlying mechanisms of the condition or syndrome remain elusive.
The study findings did not find evidence by symptoms, blood investigations or MRI to clearly define Long COVID subtypes.
The study team observed symptom recovery at 12 months in 30% of individuals with Long COVID, particularly with cardiopulmonary and systemic symptoms, aligning with other longitudinal studies.
However, the findings of reductions in HRQoL and time at work reinforce prior research and are concerning, despite improvement over time. Future research must consider associations between symptoms, multi-organ impairment and function in larger cohorts, enabling clearer stratification and evaluation of treatments.
In the meantime, with the new BA.2 variant and its emerging subvariants which are even more transmissible by between 30 to 50 times than the original Omicron variant spreading globally and causing new surges, it will be fun as more people get exposed and infected with the virus while more stupid and ignorant doctors and media keep on saying that we do not have to be worried about this new surges not knowing or understanding the long term health implications and life spans being shortened when one gets exposed to the virus.
https://www.washingtonpost.com/opinions/2022/03/21/ba2-covid-wave-concerns-restrictions/
Hopefully, the excess death rates in coming months and years in countries like United Kingdom, Singapore, Thailand, India, China along with those controlling the COVID-19 narratives in the United States etc will be exponential and hopefully many of the ignorant/stupid and those living in denial will suffer both economically and painfully before succumbing to fatal outcomes.
For more on the
SARS-CoV-2 and shortened life spans, keep on logging to Thailand
Medical News.