BREAKING! Colorado Scientist identify New Gut Bacterial Arthritogenic Strain From The Subdoligranulum Genus That Causes Rheumatoid Arthritis!
Source: Medical News - Arthritis Oct 31, 2022 3 years, 1 month, 3 weeks, 1 day, 6 hours, 33 minutes ago
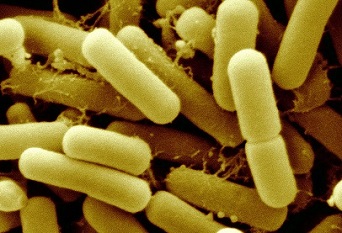
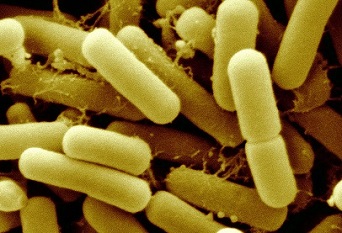
Scientists form the University of Colorado Anschutz Medical Campus – USA have made a startling discovery in which they identified a new strain of gut bacteria from the Subdoligranulum genus that is arthritogenic and able to cause Rheumatoid Arthritis!
The study also involved researchers from Stanford University School of Medicine, California - USA and Benaroya Research Institute, Seattle - U.S.A.
The mucosal origins hypothesis of rheumatoid arthritis (RA) proposes a central role for mucosal immune responses in the initiation or perpetuation of the systemic autoimmunity that occurs with disease.
To date however, the connection between the mucosa and systemic autoimmunity in RA remains unclear.
Utilizing dual immunoglobulin A (IgA) and IgG family plasmablast–derived monoclonal autoantibodies obtained from peripheral blood of individuals at risk for rheumatoid arthritis (RA), the study team identified cross-reactivity between RA-relevant autoantigens and bacterial taxa in the closely related families Lachnospiraceae and Ruminococcaceae.
After generating bacterial isolates within the Lachnospiraceae/Ruminococcaceae genus Subdoligranulum from the feces of an individual, the study team confirmed monoclonal antibody binding and CD4+ T cell activation in individuals with RA compared to control individuals.
Furtnermore, when Subdoligranulum isolate 7 but not isolate 1 colonized germ-free mice, it stimulated TH17 cell expansion, serum RA–relevant IgG autoantibodies, and joint swelling reminiscent of early RA, with histopathology characterized by antibody deposition and complement activation. Systemic immune responses were likely due to mucosal invasion along with the generation of colon-isolated lymphoid follicles driving increased fecal and serum IgA by isolate 7, because B and CD4+ T cell depletion not only halted intestinal immune responses but also eliminated detectable clinical disease. In aggregate, these findings demonstrate a mechanism of RA pathogenesis through which a specific intestinal strain of bacteria can drive systemic autoantibody generation and joint-centered antibody deposition and immune activation.
Autoantibodies can be detected in individuals at risk for developing rheumatoid arthritis (RA) before development of clinical disease. The source of these autoantibodies, however, remains unclear.
Past studies identified that IgG and IgA autoantibodies from individuals who are at risk for RA cross-react against gut bacteria in the Lachnospiraceae and Ruminococcaceae families.
Interestingly, further analysis identified a new bacterial strain from the Subdoligranulum genus that was associated with autoantibody development. Mice colonized with this Subdoligranulum isolate developed arthritis with pathology similar to human RA.
The study findings suggest that this Subdoligranulum strain may be a major contributor to RA autoantibody development.
The study findings were published in the peer reviewed journal: Science Translational Medicine.
https://www.science.org/doi/10.1126/scitranslmed.abn5166
The study findings are among the first that shows a new unique bacteria found in the gut could be responsible for triggering rheumatoid arthritis (RA) in individuals already at risk fo
r the autoimmune disease.
Dr Kristine Kuhn, MD, Ph.D., associate professor of rheumatology, led a team of scientists from the Division of Rheumatology on the study along with post graduate student Dr Meagan Chriswell who is the lead author of the paper.
Dr Kuhn told Thailand
Medical News, "Previous work led by co-authors Dr Kevin Deane, Dr Kristen Demoruelle, and Dr Mike Holers here at Colorado Univeristy helped establish that we can identify individuals who are at risk for rheumatoid arthritis (RA) based on serologic markers, and that these markers can be present in the blood for many years before diagnosis.
Dr Kuhn further added, “When they looked at those antibodies, one is the normal class of antibody we normally see in circulation, but the other is an antibody that we usually associate with our mucosa, whether it be the oral mucosa, the gut mucosa, or the lung mucosa. We started to wonder, 'Could there be something at a mucosal barrier site that could be driving RA?'"
The study team with the help of a group led by Dr Bill Robinson, MD, Ph.D., at Stanford University, took the antibodies created by immune cells from individuals whose blood markers showed they were at risk for the disease and mixed them with the feces of the at-risk individuals to find the bacteria that were tagged by the antibodies.
In order to further test their hypothesis, the study team used animal models to host the newly discovered bacteria. Those experiments showed that not only did the bacteria cause the animal models to develop the blood markers found in individuals at risk for RA; but some of the models showed development of full-blown RA as well.
Dr Kuhn said, "Our collaborators led by Dr Eddie James and Dr Jane Buckner of Benaroya Research Institute confirmed that the T cells in the blood of individuals with RA will respond to these bacteria, but individuals who are otherwise healthy do not respond to these bacteria.”
Dr Kuhn explained, “Through studies in humans and animal models, we were able to identify these bacteria as being associated with the risk for developing RA. They trigger an RA-like disease in the animal models, and in humans, we can show that this bacterium seems to be triggering immune responses specific to RA."
Dr Kuhn stressed that if the new unique species of bacteria is indeed driving the immune response that leads to RA in individuals already at risk for the disease, it might be possible to target the bacteria with medication to prevent that response from happening.
She added, "The next thing we want to do is identify, in larger populations of individuals at risk for RA, if these bacteria correlate with other genetic, environmental, and mucosal immune responses, and then ultimately, the development of RA. Then we could say, 'This is a marker that's useful in helping predict who will go on to develop RA,' and apply prevention strategies. The other opportunity there is that if we can understand how, it is triggering these immune responses, we might be able to block the bacteria's ability to do that."
The study took five years to conduct and analyze, Dr Kuhn says, helped along by individuals who discovered they were at risk for RA and volunteered to support the research effort. Eventually the researchers want to examine exactly how the bacteria triggers the immune response, as well as different methods of preventing the reaction from happening.
She said, "There are a lot of different technologies that are just starting to come out that could selectively target a bacterium in the gut microbiome, for example, to prevent it from having immunogenic effects on the host. For a long time, people have thought that antibiotics could be a useful therapy for RA, but rather than the sledgehammer effect of a traditional antibiotic that's going to wipe out a large group of bacteria, we might be able selectively target this bacterium or its effects."
For more about
Arthritis, keep on logging to Thailand
Medical News.