BREAKING! COVID-19 Antibodies: Dutch Researchers Warn That COVID-19 Antibody Therapies Containing IgG Could Backfire Badly In Patients
Source: COVID-19 Antibodies Jul 15, 2020 5 years, 5 months, 1 week, 3 days, 3 hours, 42 minutes ago
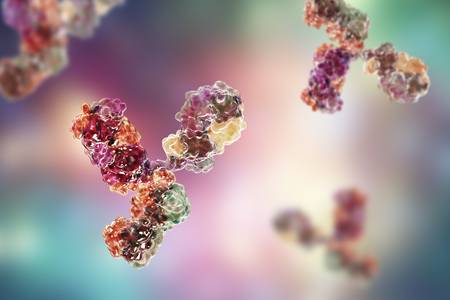
COVID-19 Antibodies: A new study by researchers from Netherlands warns against the use of any COVID-19 therapies containing the IgG antibodies as these would react with the macrophages in the bodies of the infected and accelerate cytokine storms.
Though these IgG antibodies are more prevalent in large amounts in patients with severe COVID-19 conditions, they are also found in very small amounts in the blood plasma of those who have recovered.
The research findings are published on a preprint server but are currently being peer reviewed.
https://www.biorxiv.org/content/10.1101/2020.07.13.190140v1
The hyperactive immune system is characterized by high levels of cytokines that promote inflammation, including IL-6, IL-8, and TNF. On the other hand, early response antiviral cytokines like type I and III interferons (IFNs) are suppressed. The combination of low antiviral response with high pro-inflammatory cytokine levels causes a very unfavorable immune response in severe COVID-19.
The study aimed to examine the possibility that the anti-spike IgG antibodies are behind the excessive inflammation in these patients. These IgG antibodies used macrophages induced to present the M2 phenotype and exposed them to spike-IgG a well as to the viral mimic PolyIC.
Although individually, these stimuli produced low levels of IL-1β, IL-6, and TNF, and high levels of IL-8, vs. hardly any cytokine secretion, respectively, combined stimulation caused a steep increase in the secretion of IL-1β, IL-6, and TNF. These are associated with severe COVID-19. IL-10 secretion also surged though it is an anti-inflammatory cytokine. The researchers then confirmed the findings using primary lung macrophages.
In order to further trace the cause of this inflammation, they looked at serum from 33 patients in the intensive care unit (ICU) who fell into one of three categories: 1) No COVID-19. 2) COVID-19 positive but anti-spike IgG negative and 3) COVID-19 positive and anti-spike IgG positive.
The research team found that as expected, the cytokines mentioned earlier were secreted at much higher levels in the third group. Follow-up RNA sequencing of macrophages stimulated with the serum from the patients in the third group also indicated that pro-inflammatory genes were being induced, but also IFN-β and IFN-γ. Further analysis showed that the enhanced macrophage secretion of these cytokines was associated with anti-spike IgG in a dose-dependent manner.
Dr Jeroen den Dunnen, corresponding author from the Department of Rheumatology and Clinical Immunology, Amsterdam UMC, University of Amsterdam, told Thailand Medical News, “These data demonstrate that anti-Spike IgG immune complexes generated from the serum of severely ill COVID-19 patients induce a strong pro-inflammatory response by (otherwise immunosuppressive) human M2 macrophages, which is characterized by high production of classical cytokine storm mediators such as IL-1β, IL-6, IL-8, and TNF.”
Also discovered by the researches was the fact that there is pulmonary edema due to the breakdown of the endothelium of the small blood vessel. Coagulation abnormalities are also found, including lung clots
. The study team found that rather than exposure to PolyIC, which caused only a brief reduction in endothelial barrier strength, the combined stimulation of endothelium with spike protein and the serum from severe COVID-19 patients caused sustained disruption of the barrier, and increased adhesion of platelets to vascular endothelium.
The endothelium also released von Willebrand factor, which indicates procoagulability. Thus, the anti-spike IgG found in the serum of patients with severe COVID-19 causes not only macrophage-mediated hyperinflammation but enhanced damage to the microvascular endothelium and clots within the smallest blood vessels.
The study team also found that the glycosylation pattern of the anti-spike IgG contributes to the strongly pro-inflammatory nature of these antibodies because the recombinant IgG fails to produce this level of stimulation. In fact, a reduction in the fucose content with an increase in galactose is a hallmark of anti-spike IgG1, compared to the sugar residue content of total IgG in the same patients.
Interestingly, the lower the fucose content, the higher was the production of IL-1β, IL-6, and TNF, but not IL-8 and IL-10. This low-fucose high-galactose pattern was then simulated in COVAI-18 to confirm that this was indeed the cause of the increased induction of pro-inflammatory cytokines.
Dr Jeroen den Dunnen commented, “These data indicate that anti-Spike IgG from COVID-19 patients has an aberrant glycosylation pattern that makes these antibodies intrinsically more inflammatory than ‘common’ IgGs by increasing its capacity to induce high amounts of pro-inflammatory cytokines.”
The researchers also examined different means of counteracting these antibodies. They first found that these anti-SARS-CoV-2 IgG immune complexes bound to
Fc gamma receptors (FcγRs), which are highly expressed on human macrophages. By selectively blocking each type of FcγR, they found that though all induced anti-spike IgG-mediated inflammation, this effect was most apparent with FcγRII. The low-fucose, high-galactose combination of sugars on the anti-spike IgG especially increases the affinity of the antibody for FcγRIII, but this is not the most prominent contributor to the hyperinflammatory response in severe COVID-19.
These FcγRs are expressed by other cells, including human airway epithelium, which not only interacts closely with activated macrophages but presents a primary target for SARS-CoV-2.
The FcγR-signaling pathway depends on the kinase enzyme Syk, and blockade of this using an active form of
fostamatinib, a small molecule inhibitor, produced virtually complete inhibition of secretion of these cytokines induced by anti-spike IgG but not those induced by PolyIC stimulation alone.
Interestingly at the gene level, the study team found this small molecule suppressed over 4,300 genes, and almost 4,000 genes were upregulated. Many of the suppressed genes encoded pro-inflammatory cytokines. Thus, “these data demonstrate that the excessive inflammatory response by anti-Spike IgG from severely ill COVID-19 patients can be counteracted by the Syk inhibitor fostamatinib.”
The compound Fostamatinib may also inhibit the expression of Mucin-1 on epithelial cells, according to a recent study. This could mean that multiple pathways of inflammation are inhibited simultaneously.
The study contributes to explaining why severe COVID-19 disease often occurs around the time of activation of adaptive immunity. Other molecules involved in FcγR signaling could be targeted by other drugs as well. Again, FcγR stimulation induces human macrophages to undergo metabolic reprogramming. This could be yet another potential drug target.
These research findings thus offer several clues towards the identification of therapies to suppress these hyperinflammatory phenomena and promote recovery from serious COVID-19 illness. Moreover, it may indicate that the aberrantly glycosylated IgGs found in the serum of convalescent COVID-19 patients who were severely ill should be filtered out before using the serum to treat other patients.
For more on
COVID-19 Antibodies , keep on logging to Thailand Medical News