BREAKING COVID-19 News! SARS-CoV-2 Can Lead To Brain Calcification, Causing Neurodegenerative, Neuropsychiatric And Movement Issues And Also Seizures!
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 10, 2023 2 years, 2 months, 3 weeks, 1 day, 14 hours, 46 minutes ago
COVID-19 News: In an alarming discovery via meta-analysis of various published studies and case reports, it has been has discovered that SARS-CoV-2 infections can lead to brain calcifications,…. which in rare cases, develop rapidly over a short period of time but in most cases…over a long period of time after an individual has got exposed to the SARS-CoV-2 virus!
More emerging studies, cases reports and
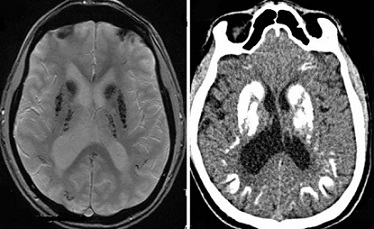
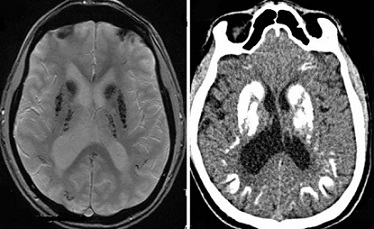
COVID-19 News reports of late has shown that exposure to the SARS-CoV-2 virus can result in the development of Fahr's syndrome - a rare neurological disorder characterized by abnormal deposits of calcium in areas of the brain that control movement, including the basal ganglia and the cerebral cortex. Symptoms of the disorder may include deterioration of motor function, neurodegenerative and neuropsychiatric issues as well as seizures.
While Fahr’s Syndrome itself has always been a genetically dominant, inherited neurological disorder, it is not known if the SARS-CoV-2 virus is triggering epigenetic changes in the human host to cause this condition. More detailed studies are urgently warranted on this.
A number of case reports and studies have already confirmed the cerebral calcification seen in SARS-CoV-2 infected patients and also in post COVID patients.
https://link.springer.com/article/10.1007/s10072-020-04733-7
https://academic.oup.com/jcemcr/article/1/3/luad072/7209242
https://scholar.unair.ac.id/en/publications/secondary-fahrs-disease-a-differential-to-be-considered-in-a-covi
https://www.cureus.com/articles/93800-the-impact-of-covid-19-infection-on-a-neurologically-compromised-male-with-fahrs-disease-presenting-with-acute-delirium-and-aspiration-pneumonia-a-case-report#!/
https://www.neurology-asia.org/articles/neuroasia-2020-25(4)-607.pdf
https://www.hippokratia.gr/2023/07/19/incidental-diagnosis-of-fahrs-syndrome-after-coronavirus-disease-2019-infection-with-the-fatal-outcome/
https://journals.sagepub.com/doi/pdf/10.1177/02537176211072256
https://onlinelibrary.wiley.com/doi/10.1111/nan.12662
;
https://journals.lww.com/oncology-times/fulltext/2023/01050/mri_shows_brain_abnormalities_in_post_covid.20.aspx
Symptoms of the Fahr's syndrome may include:
-Deterioration of motor function
-Dementia
-Seizures
-Headache
-Dysarthria (poorly articulated speech)
-Spasticity (stiffness of the limbs)
-Spastic paralysis
-Eye impairments
-Athetosis (involuntary writhing movements)
Fahr's syndrome can also include symptoms characteristic of Parkinson's disease such as:
-Tremors
-Muscle rigidity
-A mask-like facial appearance
-Shuffling gait
-A "pill-rolling" motion of the fingers
These symptoms generally occur later in the development of the disease. More common symptoms include:
-Dystonia (disordered muscle tone)
-Chorea (involuntary rapid, jerky movements)
Major Neurocognitive Disorder (NCD) is a complex condition with a wide range of potential causes, often remaining unspecified. Fahr's syndrome (FS) is a rare neurodegenerative disorder that manifests with diverse neurological, neuropsychiatric, and movement-related symptoms. FS is characterized by bilateral basal ganglia calcifications, typically resulting from other underlying conditions such as endocrine and metabolic disorders or infectious diseases
In the recent case study published in the peer reviewed journal: Archives of Clinical Neuropsychology on the 8
th of October 2023, researchers detailed the case of a 75-year-old patient.
https://academic.oup.com/acn/advance-article-abstract/doi/10.1093/arclin/acad067.121/7299836
Case Description: A 75-year-old Caucasian male sought neuropsychological assessment following concerns raised by his spouse regarding the sudden onset of mood disturbances, anhedonia, hypersomnia, disinhibition, and unusual motor behaviors, which had begun two years prior and worsened after he contracted COVID-19. The patient had a history of multiple comorbid medical conditions, including hypothyroidism, hypercholesterolemia, intermediate hyperglycemia, prostate cancer (in remission), and a previous syncopal episode. Neuroimaging revealed bilateral basal ganglia calcifications and white matter lesions.
Results: During the examination, the patient displayed hypomimia (reduced facial expression), an ataxic gait, alogia (difficulty in finding words), sporadic motor stereotypies (repetitive movements), and motor overflow (involuntary muscle contractions). His overall performance on the Meyers Neuropsychological Battery was rated as Below Average, with particular weaknesses in attention, memory, processing speed, mental flexibility, and motor function. The patient received a diagnosis of Major NCD with an unspecified etiology and was advised to continue consultations with a neurologist.
Conclusions: The cognitive difficulties observed in this patient appear to have multiple contributing factors, likely stemming from a combination of basal ganglia calcification, white matter changes, hypothyroidism, and the prior COVID-19 infection, suggesting a possible diagnosis of Fahr’s syndrome (FS). This case underscores the importance of considering various potential causes, including the effects of COVID-19, in the diagnostic process, especially as our understanding of the neurological manifestations of the virus continues to evolve.
There are many of such cases emerging and doctors and healthcare professionals need to be attention while diagnosing patients with various neurological manifestations and also to consider the presence of Fahr’s syndrome (FS) and to check for cerebral calcifications using brain MRI.
For the latest
COVID-19 News, keep on logging to Thailand Medical News.