Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 19, 2023 1 year, 5 months, 3 days, 6 hours, 12 minutes ago
COVID-19 News: In a startling development that could reshape our understanding of the cardiovascular complications associated with COVID-19, a collaborative research effort involving prestigious institutions such as the New York University School of Medicine, Einstein Medical Center in Philadelphia, Washington University in St. Louis, SUNY Upstate in Syracuse, and Urmia University of Medical Sciences in Iran has uncovered a rare and concerning link between SARS-CoV-2 infections and Brugada Syndrome (BRS).
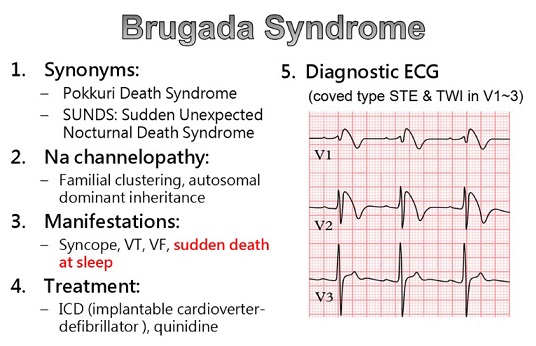
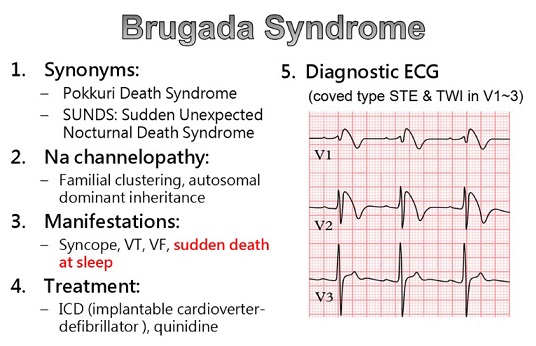
Brugada Syndrome, a relatively uncommon channelopathy characterized by distinct electrocardiogram (ECG) patterns, is known for posing an elevated risk of sudden cardiac death (SCD), even in the absence of structural heart disease. However, the most intriguing aspect of this study is its revelation of a unique case where a Brugada pattern emerged in a COVID-19 patient who did not exhibit the expected symptom of fever, challenging our conventional understanding of the relationship between COVID-19 and cardiac complications.
Thailand Medical News would however like to add that while the research team claimed that the incidence of Brugada Syndrome can be considered rare as a result of SARS-CoV-2 infections, various studies, cases reports and
COVID-19 News reports are showing that these incidences are not so rare after all. Also, it should be noted that in many cases, there is no proper comprehensive healthcare screenings for COVID-19 infected individuals both during acute infection and post-COVID stages, hence the diagnosis of Brugada syndrome might be missed.
https://academic.oup.com/ehjcr/article/5/12/ytab454/6423209
https://www.cureus.com/articles/147830-ventricular-fibrillation-in-an-afebrile-covid-19-patient-presenting-with-transient-type-i-brugada-pattern#!/
https://onlinelibrary.wiley.com/doi/10.1002/emp2.12810
https://www.journalmc.org/index.php/JMC/article/view/3644
https://www.cambridge.org/core/journals/cardiology-in-the-young/article/covid19-reveals-brugada-pattern-in-an-adolescent-patient/4ADD7BE1DC495AB775A401F12CDE4BB7
https://www.sciencedirect.com/science/article/pii/S2666084920303661
https://www.ejcrim.com/index.php/EJCRIM/article/view/1808
ent-with-covid-19-infection-associated-fever-a-case-of-brugada-pattern#!/">https://www.cureus.com/articles/34678-st-elevation-in-a-patient-with-covid-19-infection-associated-fever-a-case-of-brugada-pattern#!/
https://www.cureus.com/articles/70928-fever-and-hyponatremia-unmasking-brugada-pattern-electrocardiogram-in-a-patient-with-sars-cov-2-infection#!/
https://link.springer.com/article/10.1007/s12471-020-01459-1
https://www.mdpi.com/2308-3425/9/4/96
https://linkinghub.elsevier.com/retrieve/pii/S1878540922000056
https://onlinelibrary.wiley.com/doi/10.1111/anec.13051
To appreciate the significance of this discovery that SARS-CoV-2 infections can cause Brugada Syndrome, it is crucial to delve into the intricacies of Brugada Syndrome. Initially described in 1992, BRS is an inherited arrhythmia disorder that significantly elevates the risk of sudden cardiac death in individuals with an otherwise structurally normal heart.
Signs and symptoms that may be associated with Brugada syndrome include:
-Dizziness.
-Fainting.
-Gasping and labored breathing, particularly at night.
-Irregular heartbeats or palpitations.
-Extremely fast and chaotic heartbeat.
-Seizures.
Approximately half of Brugada cases stem from loss-of-function mutations in genes such as SCN5A and SCN10A, which encode the cardiac sodium channel. Notably, individuals with BRS often remain asymptomatic and unaware of their genetic predisposition until a critical event, such as syncope or sudden cardiac arrest, prompts diagnosis. In cases where the characteristic electrocardiographic changes manifest without a history of sudden cardiac death or related episodes, it is designated as the "Brugada pattern" rather than the full syndrome. Provocative triggers, such as febrile states, electrolyte imbalances, substance use (including alcohol or cocaine), and certain medications, are known to unveil the ECG manifestation and induce arrhythmias in patients with BRS.
Already recognized as a major complication of COVID-19, arrhythmias and conduction system abnormalities have been reported in numerous cases. However, this study cun case report introduces a new dimension to our understanding of Brugada Syndrome by highlighting its potential association with COVID-19. The emergence of a type 2 Brugada pattern in a COVID-19 patient who did not exhibit fever challenges existing assumptions about the triggers for Brugada Syndrome and raises questions about the complex interplay between the virus and the cardiovascular system.
The case under scrutiny involves a male patient in his 40s with a medical history significant for diabetes and hypertension. Initially presenting to the emergency department with a one-week history of fever, chills, and headache, he tested positive for COVID-19 through reverse transcriptase polymerase chain reaction (RT-PCR) on a nasal swab. Despite stable vital signs and clinical condition, the patient was discharged. However, two days later, he returned with dyspnea on exertion, shortness of breath, and worsening symptoms. Notably, he was afebrile on this occasion. An ECG obtained during this visit revealed ST elevation in precordial leads indicative of the type 2 Brugada pattern, a surprising finding given the absence of fever.
Further investigation through a chest X-ray demonstrated diffuse interstitial and patchy ground-glass opacities consistent with COVID pneumonia. A subsequent CT scan of the chest ruled out pulmonary emboli but confirmed multi-lobar pneumonia. Importantly, the patient's echocardiogram displayed normal findings with no structural or valvular abnormalities, and there was no pericardial effusion. Despite concerns for an ST elevation myocardial infarction (STEMI), coronary angiography revealed clear coronary arteries.
The patient's laboratory results were largely within normal limits, except for elevated markers such as creatinine, ferritin, and lactate dehydrogenase. Notably, the persistence of a positive COVID-19 test underscored the relevance of the viral infection in the context of cardiac abnormalities.
This unprecedented case prompts a reevaluation of the understanding of COVID-19's impact on the cardiovascular system, specifically its potential role in inducing Brugada patterns. The absence of fever in this patient challenges established triggers for Brugada Syndrome, opening avenues for further research into the intricate relationship between SARS-CoV-2 and cardiac arrhythmias.
This groundbreaking research conducted by collaborative efforts from renowned medical institutions sheds light on a previously unrecognized aspect of COVID-19's impact on the cardiovascular system. The revelation that SARS-CoV-2 infections may induce Brugada patterns, even in the absence of fever, warrants careful consideration and further exploration. As the scientific community delves deeper into the intricacies of COVID-19, this case serves as a poignant reminder of the multifaceted nature of the virus and the imperative for ongoing research to unravel its diverse manifestations.
Moving forward, it is essential to expand this research to a larger cohort of COVID-19 patients to ascertain the prevalence of Brugada patterns and understand the underlying mechanisms. Additionally, investigating whether certain genetic predispositions in COVID-19 patients make them more susceptible to Brugada Syndrome could provide valuable insights. The implications of this discovery extend beyond the immediate clinical management of COVID-19 patients to the long-term monitoring and care of individuals who may develop Brugada patterns as a consequence of the viral infection.
Furthermore, healthcare professionals should be vigilant about the potential cardiac complications in COVID-19 patients, even in the absence of classical symptoms such as fever. Routine baseline ECGs for individuals diagnosed with COVID-19 could become a standard practice to detect any underlying cardiac abnormalities, allowing for timely intervention and management. This case emphasizes the need for a multidisciplinary approach involving cardiologists, infectious disease specialists, and geneticists to comprehensively understand and address the diverse manifestations of COVID-19.
In conclusion, the nexus between COVID-19 and Brugada Syndrome revealed in this study marks a paradigm shift in our understanding of the virus's impact on the cardiovascular system. The intricate interplay between viral infections, genetic predispositions, and cardiac arrhythmias demands meticulous exploration. As we navigate the evolving landscape of COVID-19 research, this case serves as a beacon, guiding future investigations toward a more comprehensive understanding of the virus's diverse effects on the human body.
The study findings cum case report was published in the peer reviewed journal: Acta Medica.
https://actamedica.lfhk.cuni.cz/66/2/0068/
For the latest
COVID-19 News, keep on logging to Thailand Medical News