Breaking COVID-19 News! Scientists Discover Potentially New Fatal Complication Of SARS-Cov-2 Infection - Pulmonary Fat Embolism!
Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 05, 2023 2 years, 4 months, 1 day, 5 hours, 50 minutes ago
COVID-19 News: As the COVID-19 pandemic continues to disrupt lives worldwide, researchers remain vigilant in uncovering the multifaceted impact of the SARS-CoV-2 virus. Beyond the widely recognized respiratory symptoms and complications, there lies a potential hidden danger: Pulmonary Fat Embolism (PFE).
Researchers from the Southern Medical University-China and the Forensic Department of Criminal Investigation Bureau - China have in a new study and cases study delved into the groundbreaking discovery of Pulmonary Fat Embolism or PFE as a new and potentially fatal complication of SARS-CoV-2 infection, shedding light on a case that may transform our understanding of the virus's impact on the human body.
The Global COVID-19 Landscape
Since its initial outbreak in December 2019, the SARS-CoV-2 virus has swept across the globe with unprecedented speed. According to
COVID-19 News updates, as of August 31st 26, 2023, there has been more than 765 million confirmed cases and over 6.95 million deaths. These staggering numbers underscore the urgent need for a deeper understanding of the virus's various implications on human health.
Common Causes of COVID-19-Related Deaths
While COVID-19 primarily manifests as a respiratory illness, it has been associated with a range of severe complications, including diffuse alveolar injury and acute respiratory distress syndrome. In many cases, these complications directly contribute to patients' demise. Notably, autopsy results have revealed a concerning trend - 80-100% of COVID-19 patients exhibit microthrombi, a nine-fold increase compared to influenza patients. This finding underscores the critical role of thrombus formation in COVID-19 fatalities.
The Emergence of Pulmonary Fat Embolism
Although fat embolism has been reported in some COVID-19 cases, investigations into its epidemiology and its potential as a fatal complication have been lacking.
In this new report, the study team present a groundbreaking case that highlights the emergence of Pulmonary Fat Embolism (PFE) as a life-threatening consequence of SARS-CoV-2 infection.
Case Presentation
The case in question involved a 54-year-old woman who experienced sudden illness while at work. She struggled to breathe for 40 minutes and subsequently lost consciousness for 20 minutes before being admitted to the hospital. Upon arrival, her body temperature was normal, but she exhibited undetectable respiration, heart rate, and blood pressure. Despite immediate medical intervention, including cardiopulmonary resuscitation and other life-saving measures, she was declared clinically dead within two hours of admission. The initial suspicion was that of sudden cardiac death.
Autopsy Reveals Alarming Findings
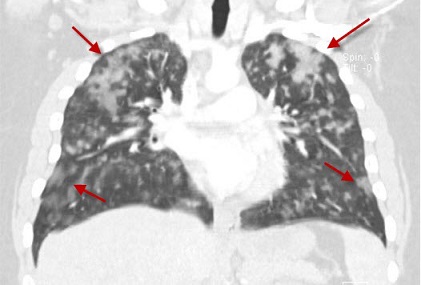
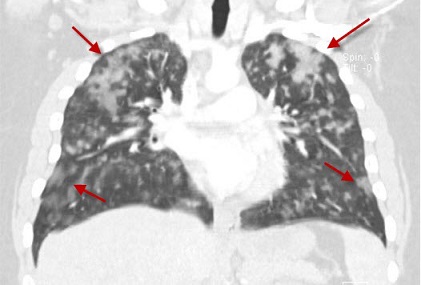
A forensic autopsy conducted two days after her death uncovered striking anomalies. Externally, no fatal trauma beyond rescue-related marks was evident. However, the bilateral thorax contained approximately 50 mL of light red fluid, while both lungs were congested a
nd oedematous, with the left lung weighing 600 g and the right lung weighing 700 g. Intriguingly, no lethal pathological changes were observed in other organs.
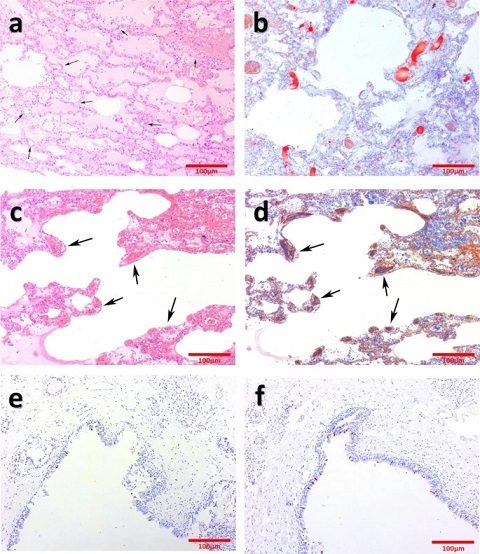
Histopathological examination, particularly hematoxylin and eosin (HE) staining, exposed severe pulmonary oedema and pulmonary haemorrhage in both lungs. Suspicion arose when microthrombi and vacuolar structures were discovered within the lumen of numerous small pulmonary interstitial vessels. Further staining with phosphotungstic acid hematoxylin (PTAH) and oil red O (ORO) confirmed the presence of Pulmonary Fat Embolism (PFE) and microthrombi.
Immunohistochemistry of the spike protein and nucleocapsid protein corroborated SARS-CoV-2 infection, providing a critical link between the virus and Pulmonary Fat Embolism or PFE.
Microthrombus Embolism in COVID-19
The relationship between SARS-CoV-2 and microthrombus embolism has been a focal point of research due to its significant contribution to COVID-19 mortality.
Studies have shown that alveolar capillary microthrombi occur at a rate nine times higher in COVID-19 patients than in those with influenza. Furthermore, autopsy findings indicate that microthrombi are present in 80-100% of COVID-19 cases.
D-dimer, a key marker for thrombus formation, has also emerged as an important indicator in predicting the outcome of COVID-19 patients. Elevated D-dimer levels have been correlated with fatal pulmonary embolism in COVID-19 patients. In the case presented here, the patient's high D-dimer levels, combined with histopathological evidence of microthrombus embolism, underscored the role of hypercoagulation in COVID-19 fatalities.
Understanding Pulmonary Fat Embolism
Fat embolism, a phenomenon characterized by lipid droplet occlusion in microvascular or capillary networks, has long been studied in the context of trauma-related injuries. The presence of fat droplets in the lungs was first described in 1861, and subsequent research has advanced both mechanical and biochemical theories to explain its occurrence. Recent investigations have suggested that elevated C-reactive protein (CRP) levels, an inflammatory marker, may contribute to the formation of fat emboli. In the case at hand, the patient exhibited an exceptionally high CRP level (26.55 mg/L) before death, pointing towards a possible link between SARS-CoV-2 infection and elevated CRP in the development of Pulmonary Fat Embolism (PFE).
Exploring Potential Mechanisms
Intriguingly, while one theory suggests that PFE may result from visceral fat necrosis and the transfer of free fat droplets into circulation in obese COVID-19 patients, this particular case did not provide evidence of SARS-CoV-2 infection in the adipose tissue surrounding vital organs. Thus, the exact mechanisms underlying SARS-CoV-2-induced PFE remain an area of active investigation.
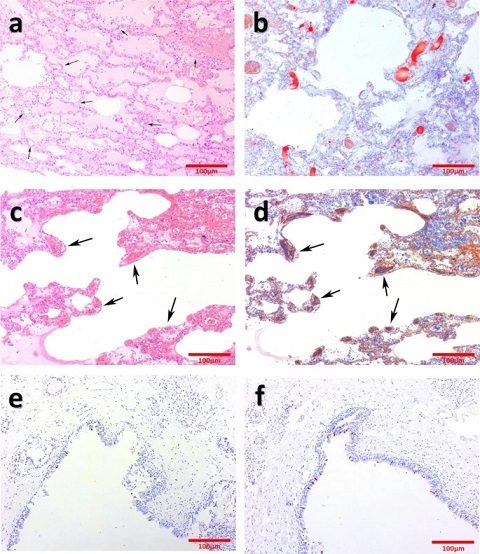 a: Diffuse pulmonary oedema, pulmonary haemorrhage and vacuole structure. (HE staining, arrows). b: Grade III fatal fat embolism in pulmonary interstitial small vessels. (ORO staining). c and d: Extensive microthrombus in pulmonary interstitial small vessels. (PTAH staining, arrows). e and f: Immunohistochemistry staining of S protein (E) and N protein (F)
Challenges in Diagnosis
a: Diffuse pulmonary oedema, pulmonary haemorrhage and vacuole structure. (HE staining, arrows). b: Grade III fatal fat embolism in pulmonary interstitial small vessels. (ORO staining). c and d: Extensive microthrombus in pulmonary interstitial small vessels. (PTAH staining, arrows). e and f: Immunohistochemistry staining of S protein (E) and N protein (F)
Challenges in Diagnosis
Diagnosing Fat Embolism Syndrome (FES), the clinical manifestation of fat embolism, presents significant challenges. Several diagnostic criteria exist, including Gurd's, Schonfeld's, and Lindeque's criteria, but prospective studies with comprehensive data are lacking. Laboratory markers such as interleukin-6 (IL-6) and the presence of lipid-laden macrophages in alveolar lavage fluid have shown promise as early diagnostic indicators. Imaging techniques, although nonspecific, may also aid in diagnosis by revealing characteristic changes in lung tissue. Novel approaches, including advanced imaging methods, are essential for improved FES diagnosis.
Treatment Challenges
The treatment of FES remains a subject of debate and research. While various drug treatments have been explored, including heparin, corticosteroids, albumin, aprotinin, and hypertonic glucose, none have consistently proven effective. The management of FES remains largely supportive, and further research is needed to develop more targeted therapies.
Conclusion
In summary, the case presented here represents a pivotal discovery in our understanding of COVID-19's diverse and complex effects on the human body. Pulmonary Fat Embolism (PFE) emerges as a potentially fatal complication of SARS-CoV-2 infection, adding to the growing list of COVID-19-related complications. As the global medical community continues to grapple with this pandemic, it is crucial that clinicians remain vigilant, recognizing the potential for PFE in both acute COVID-19 cases and the emerging challenge of
The study findings were published in the peer reviewed journal: BMC Infectious Diseases.
https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-023-08559-4
For the latest
COVID-19 News, keep on logging to Thailand Medical News.