BREAKING COVID-19 News! Study Finds That Brain Demyelination Is Common In Many Post-COVID Individuals, Especially In Those With Symptoms Of Depression!
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 12, 2023 2 years, 2 weeks, 2 hours, 11 minutes ago
COVID-19 News: As the world grapples with the multifaceted aftermath of the COVID-19 pandemic, a groundbreaking study conducted by researchers from Tomsk State University in Russia, the Russian Academy of Sciences, Siberian State Medical University, and the University of Washington in Seattle, USA has unveiled a startling correlation between post-COVID depression and widespread brain demyelination. Using a state-of-the-art MRI technique known as macromolecular proton fraction (MPF) mapping, this study covered in this
COVID-19 News report, represents a significant leap forward in our understanding of the neurological consequences of COVID-19, particularly the impact on individuals experiencing post-COVID depression.
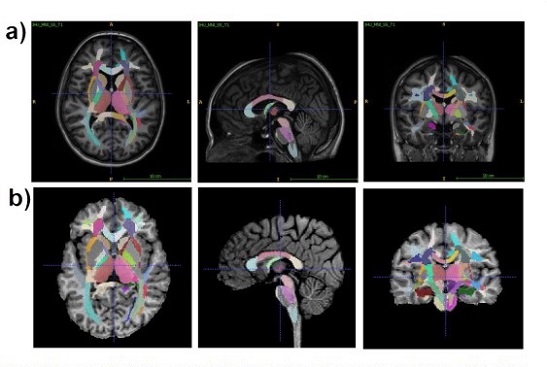
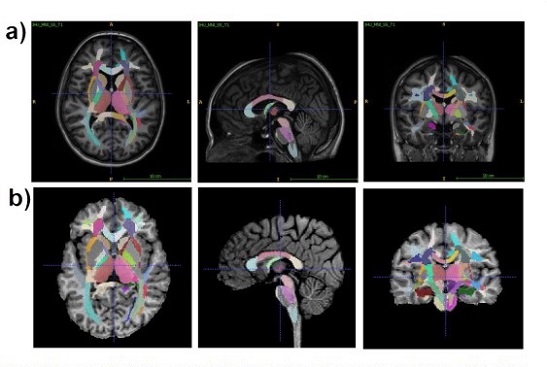 An example of T1 Eve template registration with segmentation (a) to individual MPF map (b).
An example of T1 Eve template registration with segmentation (a) to individual MPF map (b).
Slices are shown in similar axial, sagittal, and coronal projections.
The Persistence of Post-COVID Symptoms
Long-COVID syndrome, characterized by the persistence of symptoms more than 12 weeks after the acute infection, has emerged as a challenging aspect of the post-COVID landscape. Beyond the initial respiratory concerns, a spectrum of neurological and psychiatric complications has come to the fore. These include "brain fog," persistent fatigue, headaches, sleep disorders, impaired sense of smell and taste, cognitive impairment, anxiety, and notably, depression.
Depression: A Silent Threat
Among the myriad complications associated with COVID-19, depression has emerged as a silent threat, decreasing quality-of-life outcomes and potentially causing disability. Survivors of the acute phase of COVID-19 face an increased risk of being diagnosed with major depressive disorder (MDD). However, understanding the specific features of post-COVID depression (PCD) compared to traditional MDD remains a critical area of exploration. Some studies suggest differences in symptoms, with post-COVID depression displaying high levels of excitatory symptoms, possibly corresponding to a mixed form of depression.
The Inflammatory Hypothesis
The etiology of major depressive disorder is considered multifactorial, often involving the interplay of biological, genetic, environmental, and psychosocial factors. In the context of post-COVID depression, the pathological mechanisms are closely linked to inflammation triggered by the peripheral immune-inflammatory response to the viral infection. Neuroinflammation, marked by the reactivation of microglia and astrocytes, results in the release of cytokines, pro-inflammatory factors, and cytotoxic agents. This inflammatory milieu negatively affects the functions of myelinating oligodendrocytes, paving the way for demyelination.
Previous Studies on Demyelination in Post-COVID Patients
Various studies have hinted at the prevalence of white matter damage in post-COVID patients, with demyelination observed in 57% of hospitalized individuals. Additionally, reports have indicated the potential triggering of demyelinating d
iseases such as multiple sclerosis, acute disseminated encephalomyelitis, and Guillain Barré syndrome. The neurotoxic action of the virus is mediated by binding to angiotensin-converting enzyme-2 (ACE2) receptors or indirectly through the induction of a cytokine storm, disrupting the blood-brain barrier, leading to immunological mediation, increased blood coagulation, and acting as a trigger for autoimmune-mediated demyelinating injuries in the central nervous system.
The Neuroimaging Perspective
Recent MRI studies have provided a glimpse into the alterations in white matter microstructure following COVID-19 recovery, with an increase in radial diffusivity indicative of demyelination and axonal damage. Notably, major depressive disorder is often considered a disorder of white matter connectivity, rooted in changes in brain myelination. Several neuroimaging studies have demonstrated impaired white matter integrity and demyelination in patients with MDD.
MPF Mapping: A Quantum Leap in Demyelination Assessment
In this pioneering study, researchers utilized the quantitative MRI method, macromolecular proton fraction (MPF) mapping, to systematically assess demyelination in clinically diagnosed post-COVID depression. MPF mapping stands out among other MRI methods for its improved specificity to myelin and reduced susceptibility to physiological confounders. It has robust correlations with myelin content, is independent of magnetic field strength, and allows for myelin measurements across various human and animal MRI platforms.
Key Findings and Implications
The study encompassed 63 recovered COVID-19 patients at an average of 13.5 months post-recovery, including 25 identified with post-COVID depression (PCD) based on psychiatric diagnosis, and 38 in a comparison group (noPCD) with neurological COVID-19 complications, excluding clinical depression.
The MPF mapping revealed extensive demyelination in PCD patients, particularly in juxtacortical white matter, white matter tracts (including the inferior fronto-occipital fasciculus), and grey matter structures (hippocampus, putamen, globus pallidus, and amygdala).
Comparing the two groups, the PCD group exhibited more profound demyelination than the noPCD group, emphasizing the specific impact of post-COVID depression. Multiple regression analysis identified IFOF demyelination as the primary predictor of PCD presence and severity according to Hamilton scores. The number of post-COVID symptoms also emerged as a significant predictor of PCD presence, while the number of acute symptoms predicted PCD severity.
Conclusion: A New Paradigm in Post-COVID Neurology
This groundbreaking study not only marks a significant leap in our understanding of the neurological consequences of post-COVID depression but also introduces IFOF demyelination as a key biomarker. The identification of IFOF demyelination opens avenues for further research into the specific neurological impact of Sars-CoV-2 infection. As the scientific community delves deeper into the long-term consequences of the pandemic, this study serves as a critical milestone, guiding future investigations into the intricate relationship between COVID-19, neuroinflammation, and psychiatric complications. In the pursuit of clarity, future studies will illuminate whether IFOF demyelination is unique to the effects of Sars-CoV-2 or a broader characteristic of depressive disorders, shaping the landscape of post-COVID neurology.
The study findings were published on a reprint server an are currently being peer reviewed.
https://www.preprints.org/manuscript/202312.0698/v1
For the latest
COVID-19 News, keep on logging to Thailand Medical News.