BREAKING COVID-19 News! University Of California Study Finds That The Toxic Spike Proteins Of SARS-CoV-2 Causes Vascular Leaks That Leads To Various Issues!
COVID-19 News - SARS-CoV-2 Spike Proteins Causes Vascular Leaks Dec 10, 2022 3 years, 2 months, 5 days, 4 hours, 17 minutes ago
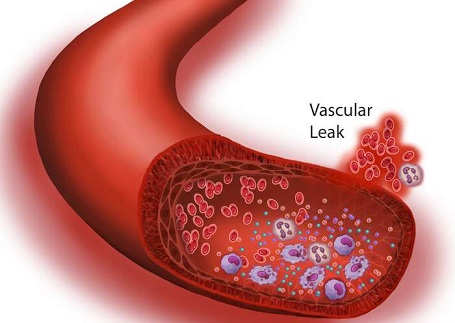
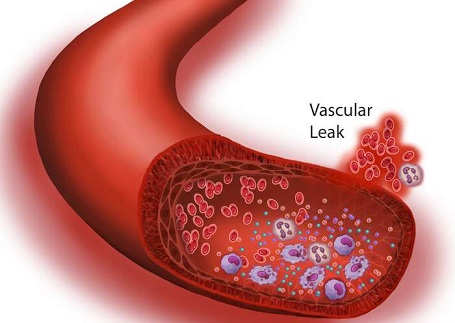
COVID-19 News: A new study by researchers from University of California – Berkeley has found that the toxic spike proteins of the SARS-CoV-2 virus are able to cause barrier dysfunction and vascular leaks in the infected, contributing to disease severity and also to various long COVID issues.
Thailand Medical News past
COVID-19 News coverages have already explained that COVID-19 is but a microvascular and endothelial disease that causes numerous health and medical issues in all exposed to the toxic spike proteins of the SARS-CoV-2 virus and also its other viral proteins.
https://www.thailandmedical.news/news/must-read-covid-19-is-nothing-but-a-microvascular-and-endothelial-disease-that-kills-fast-or-slowly-depending-on-the-human-host-health-status
https://www.thailandmedical.news/news/stellenbosch-university-study-finds-that-long-covid-is-caused-by-the-increased-levels-of-six-inflammatory-molecules-triggering-thrombotic-endotheliiti
https://www.thailandmedical.news/news/university-of-texas-study-findings-validates-that-sars-cov-2-spike-protein-causes-endothelial-vascular-dysfunction
https://www.thailandmedical.news/news/covid-19-endotheliopathy-yale-researchers-finds-that-early-detection-of-blood-vessel-injury-via-diagnostics-critical-to-predicting-survival-in-covid-1
https://www.thailandmedical.news/news/israeli-scientist-identify-nsp2,-nsp5-c145a-and-nsp7-as-key-sars-cov-2-proteins-that-damage-human-host-endothelial-cells-of-blood-vessels
https://www.thailandmedical.news/news/must-read-covid-19-swiss-research-indicates-that-sars-cov-2-coronavirus-attacks-the-lining-of-blood-vessels-across-the-body-in-severe-covid-19-stages
https://www.thailandmedical.news/news/covid-19-news-briefs-study-warns-lung-damage-continues-in
-recovered-yet-another-study-shows-recovered-will-suffer-persistent-endotheliopathy
https://www.thailandmedical.news/news/covid-19-news-american-study-confirms-that-spike-proteins-of-sars-cov-2-coronavirus-is-able-to-disrupt-the-human-blood-brain-barrier
https://www.thailandmedical.news/news/breaking-irish-study-shows-that-integrins-could-be-receptors-for-sars-cov-2-and-integrin-signaling-upon-infection-leads-to-vascular-dysregulation
https://www.thailandmedical.news/news/japanese-study-finds-that-sars-cov-2-from-infected-epithelial-cells-disrupts-the-endothelial-barrier-by-downregulating-claudin-5-cldn5-a-tight-junctio
According to the study team form the University of California-Berkeley, severe COVID-19 is associated with epithelial and endothelial barrier dysfunction within the lung as well as in distal organs.
Although it is appreciated that an exaggerated inflammatory response is associated with barrier dysfunction, the triggers of vascular leak are unclear.
The study team reported that cell-intrinsic interactions between the Spike (S) glycoprotein of SARS-CoV-2 and epithelial/endothelial cells are sufficient to induce barrier dysfunction in vitro and vascular leak in vivo, independently of viral replication and the ACE2 receptor.
The study team identified an S-triggered transcriptional response associated with extracellular matrix reorganization and TGF-β signaling.
Utilizing genetic knockouts and specific inhibitors, the study team demonstrated that glycosaminoglycans, integrins, and the TGF-β signaling axis are required for S-mediated barrier dysfunction.
Importantly, the study findings showed that SARS-CoV-2 infection caused vascular leaks in vivo, which was reduced by inhibiting integrins.
The study findings offer mechanistic insight into SARS-CoV-2-triggered vascular leak, providing a starting point for development of therapies targeting COVID-19.
The study findings were published in the peer reviewed journal: Nature Communications.
https://www.nature.com/articles/s41467-022-34910-5
The study is the first to show how a viral toxin produced by the SARS-CoV-2 virus may contribute to severe COVID-19 infections.
The research findings show how a portion of the SARS-CoV-2 Spike protein can damage cell barriers that line the inside of blood vessels within organs of the body such as the lungs, contributing to what is known as vascular leak.
Importantly, blocking the activity of this protein may help prevent some of COVID-19's deadliest symptoms, including pulmonary edema, which contributes to acute respiratory distress syndrome (ARDS).
Lead author, Dr Scott Biering, a postdoctoral scholar at the University of California, Berkeley told
COVID-19 News reporters, "In theory, by specifically targeting this pathway, we could block pathogenesis that leads to vascular disorder and acute respiratory distress syndrome without needing to target the virus itself. In light of all the different variants that are emerging and the difficulty in preventing infection from each one individually, it might be beneficial to focus on these triggers of pathogenesis in addition to blocking infection altogether."
The study findings show that the spike protein may work in tandem with the virus and the body's own immune response to trigger life-threatening symptoms.
The study team by examining the impact of the SARS-CoV-2 spike protein on human lung and vascular cells, and on the lungs of mice, was able to uncover the molecular pathways that allow the spike protein to disrupt critical internal barriers in the body.
Besides opening new avenues for the treatment of severe COVID-19, understanding how the spike protein contributes to vascular leak could shed light on the pathology behind other emerging infectious diseases.
Dr Biering further added, "We think that a lot of viruses that cause severe disease may encode a viral toxin. These proteins, independent of viral infection, interact with barrier cells and cause these barriers to malfunction. This allows the virus to disseminate, and that amplification of virus and vascular leak is what triggers severe disease. I'm hoping that we can use the principles that we've learned from the SARS-CoV-2 virus to find ways to block this pathogenesis so that we are more prepared when the next pandemic happens."
Typically, vascular leak occurs when the cells that line blood vessels and capillaries are disrupted, allowing plasma and other fluids to leak out of the bloodstream. In addition to causing the lung and heart damage observed in severe COVID-19, vascular leak can also lead to hypovolemic shock, the primary cause of death from dengue.
Prior to the start of theCOVID-19 pandemic, Dr Biering and other members of the Harris Research Program were studying the role of dengue virus protein NS1 in triggering vascular leak and contributing to hypovolemic shock. When the pandemic hit, the research team wondered if a similar viral toxin in SARS-CoV-2 could also be contributing to the acute respiratory distress syndrome that was killing COVID-19 patients.
Corresponding author, Dr Eva Harris from the Department of Molecular and Cell Biology, University of California added, "People are aware of the role of bacterial toxins, but the concept of a viral toxin is still a really new idea. We had identified this protein secreted from dengue virus-infected cells that, even in the absence of the virus, is able to cause endothelial permeability and disrupt internal barriers. So, we wondered if a SARS-CoV-2 protein, like spike, might be able to do similar things."
Typically, spike proteins coat the outer surface of SARS-CoV-2, giving the virus its knobby appearance. They play a critical role in helping the virus infect its hosts ie the spike protein binds to a receptor called ACE2 on human and other mammalian cells, which are like a key turning a lock and allows the virus to enter the cell and hijack cellular function. The SARS-CoV-2 virus sheds a large portion of the spike protein containing the receptor-binding domain (RBD) when it infects a cell.
Dr Biering added, "What's really interesting is that circulating spike protein correlates with severe COVID-19 cases in the clinic. We wanted to ask if this protein was also contributing to any vascular leak we saw in the context of SARS-CoV-2."
At present, researchers and scientists attribute the heart and lung damage associated with severe COVID-19 to an overactive immune response called a cytokine storm.
However, in order to test the theory that the spike protein might also play a role, Dr Biering and other team members used thin layers of human endothelial and epithelial cells to mimic the linings of blood vessels in the body. They found that exposing these cellular layers to the spike protein increased their permeability, a hallmark of vascular leak.
Utilizing CRISPR-Cas9 gene editing technology, the study team showed that this increased permeability occurred even in cells that did not express the ACE2 receptor, indicating that it could occur independently of viral infection.
Furthermore, the study team found that mice that were exposed to the spike protein also exhibited vascular leak, even though mice do not express the human ACE2 receptor and cannot be infected with SARS-CoV-2.
Lastly, with the help of RNA sequencing, the study team found that the spike protein triggers vascular leak through a molecular signaling pathway that involves glycans, integrins and transforming growth factor beta (TGF-beta). By blocking the activity of integrins, the team was able to reverse the vascular leak in mice.
Study co-author, Dr Felix Pahmeier, a graduate student in the Harris lab at University Of California Berkeley's School of Public Health commented, "We identified a new pathogenic mechanism of SARS-CoV-2 in which the spike protein can break down the barriers lining our vasculature. The resulting increase in permeability can lead to vascular leak, as is commonly observed in severe COVID-19 cases, and we could recapitulate those disease manifestations in our mouse models.”
He further added, "It was interesting to see the similarities and differences between spike and dengue virus protein NS1. Both are able to disrupt endothelial barriers, but the timelines and host pathways involved seem to differ between the two."
Although blocking the activity of integrins may be a promising target for treating severe COVID-19, Dr Harris said more work needs to be done to understand the exact role of this pathway in disease progression. While increased vascular permeability can accelerate infection and lead to internal bleeding, it can also help the body fight off the virus by giving immune machinery better access to infected cells.
Dr Francielle Tramontini Gomes de Sousa, former assistant project scientist in Harris's lab and co-first author of the study said, “SARS-CoV-2 evolved to have a spike surface protein with increased capacity of interacting with host cell membrane factors, such as integrins, by acquiring an RGD motif. This motif is a common integrin-binding factor exploited by many pathogens, including bacteria and other viruses, to infect host cells. Our research findings show how spike RGD interacts with integrins, resulting in TGF-beta release and activation of TGF-beta signaling. Utilizing in vitro and in vivo models of epithelial, endothelial and vascular permeability, we were able to improve understanding of the cellular mechanisms of increased levels of TGF-beta in COVID-19 patients and how spike-host cell interactions could contribute to disease."
The study team is continuing to study the molecular mechanisms that lead to vascular leak and is also investigating possible viral toxins in other viruses that cause severe disease in humans.
Dr Biering said, COVID-19 is not gone. We have better vaccines now, but we don't know how the virus is going to mutate in the future. Studying this process may be able to help us develop a new arsenal of drugs so that if someone is experiencing vascular leak, we can just target that. Maybe it doesn't stop the virus from replicating, but it could stop that person from dying."
The study findings also have implications in terms of Long COVID and why certain health issues and conditions manifest.
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-early-data-shows-that-new-sars-cov-2-sub-lineages-bq-1-1-and-bm-1-1-attacks-the-endothelial-cells-of-the-gut-ferociously-and-causes-disease-s
https://www.thailandmedical.news/news/ba-5-is-more-fusogenic-than-ba-1-or-ba-2-and-disrupts-respiratory-epithelial-and-endothelial-barriers-more-efficiently-and-is-more-inflammatory
https://www.thailandmedical.news/news/abstract-published-in-american-heart-association-journal-warns-that-mrna-covid-vaccines-dramatically-increases-endothelial-inflammatory-markers-and-he
https://www.thailandmedical.news/news/breaking-boston-university-discovers-that-vascular-protein-vimentin-assists-sars-cov-2-access-into-cells,-contributing-to-vascular-complications
https://www.thailandmedical.news/news/u-s-nih-study-finds-that-sars-cov-2-induced-antiphospholipid-antibodies-causes-endothelial-cell-activation-and-dysfunction-leading-to-severe-covid-19-