BREAKING! German And Swiss Study Discovers SARS-CoV-2 Targets And Causes Cellular Damage To Adrenal Glands Resulting In A Variety Of Health Conditions!
Source: Medical News Nov 23, 2021 3 years, 4 months, 4 days, 21 hours, 27 minutes ago
A new study by researchers from Germany and Switzerland has found that (SARS-CoV-2) infection can directly target and cause cellular damage to the human host adrenal glands.
The researchers from Technische Universität Dresden-Germany, University of Regensburg-Germany, University Hospital Zurich-Switzerland and the University of Zurich-Switzerland found that by targeting and causing damage to the
adrenal glands, the SARS-CoV-2 virus causes adrenal dysfunction which explains the manifestation of adrenal insufficiency in several patients infected with severe coronavirus disease 2019 (COVID-19) infection, along with some of the complications associated with long COVID.
The study findings were published in the peer reviewed journal: Diabetes And Endocrinology (By Lancet)
https://www.thelancet.com/journals/landia/article/PIIS2213-8587(21)00291-6/fulltext
The adrenal gland is an effector organ of the hypothalamic–pituitary–adrenal axis and the main source of glucocorticoids, which are critical to manage and to survive sepsis. The adrenal glands secrete a wide variety of hormones to help regulate vital processes in the body.
It was found that among other life-threatening conditions, people with severe COVID-19 illness have developed sepsis. Older adults are among the most at-risk of developing severe infection, prompting doctors to look into using adrenal steroids such as budesonide for early treatment of COVID-19 infection.
The human adrenal glands are susceptible to damage from sepsis-induced multiorgan failure. In addition, the adrenal glands’ high vascularization and blood supply can increase the risk for endothelial dysfunction and hemorrhage.
Such symptoms implying adrenal dysfunction have been observed in severe COVID-19 cases as some patients experienced endothelial damage, bilateral hemorrhages, infarctions, and sepsis-associated illness-related corticosteroid insufficiency.
https://pubmed.ncbi.nlm.nih.gov/32579380/
https://pubmed.ncbi.nlm.nih.gov/33462013/
Interestingly in a past study, researchers described patients with mild to moderate COVID-19 infections developing adrenocorticotropic hormone responses congruous with critical illness-related corticosteroid insufficiency.
https://pubmed.ncbi.nlm.nih.gov/33554871/
To date however, it remains unknown if SARS-CoV-2 indirectly or directly damaged the adrenal glands. For instance, other factors such as pituitary damage or other undiagnosed conditions such as antiphospholipid syndrome may directly cause adrenal dysfunction.
The study team sought to find the root of adrenal damage in COVID-19 infections and whether SARS-CoV-2 directly or indirectly caused it.
The study team studied adrenal gland tissues from 40 patients who died from COVID-19 illness in
Germany or Switzerland.
In the study findings, six cases had low density, and 13 cases had high-density cases of cellular damage and frequent small vessel vasculitis called endothelins in their periadrenal fat tissue. About 10 cases showed milder instances of adrenal parenchyma, and one case had a moderate version of it.
However, the study team did not find any evidence of thrombi formation, widespread hemorrhages, or degradation of adrenocortical cells.
Interestingly in 38 of the 40 cases, the team observed enhanced perivascular lymphoplasmacellular infiltration of different densities and sporadically mild extravasation of erythrocytes.
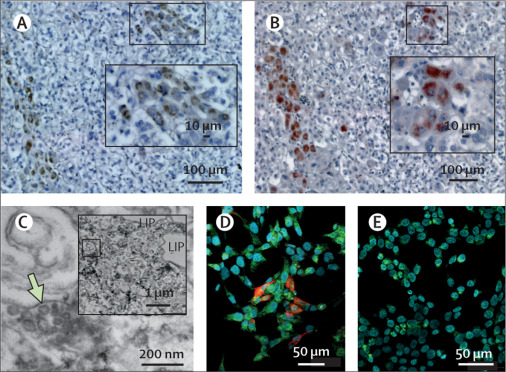
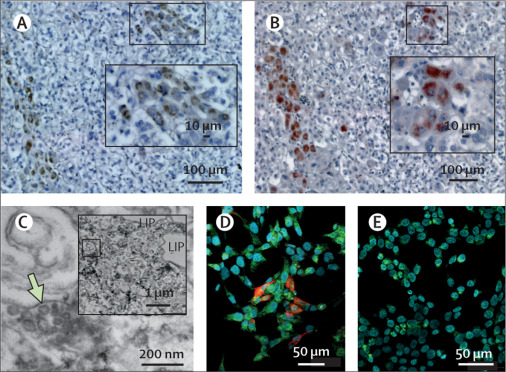 (A) Detection of SARS-CoV-2 RNA by in situ hybridization (ISH; brown DAB staining) and (B) its spike protein by immunohistochemistry (red AEC staining) was found in the same region of two serial 1 μm-thick tissue sections of the adrenal gland. Inserts depict the same regions but were captured at lower magnification showing the chosen area of virus positivity (white squares). Scattered expression of either mRNA or protein can be found in the inner parts of the adrenal gland cortex close to the medulla. Scale bars in pictures from panel A and B represent 100 μm (10 μm in the insert image). (C) Ultrastructural examination of a SARS-CoV-2 triple positive (ISH, immunohistochemistry, and RT-qPCR) adrenal tissue showing numerous viral-like particles in liposome (LIP)-rich adrenocortical cells. A scale bar represents 200 nm. A low magnification picture shown in the insert depicts the region of interest indicated by a green arrow in the enlarged picture. Scale bar in insert indicates 1 μm distance. (D) A positive immunofluorescent red signal (CY3) indicating the expression of spike protein in SARS-CoV-2 infected human adrenocortical cells. (E) Lack of positive signal (CY3) in mock-infected control cells. Adrenocortical cells were additionally stained with an antibody against side-chain cleavage enzyme (CYP11A1), which is a steroidogenic marker (green signal; CY5). Nuclei were counterstained with Hoechst 33342 dye (blue signal). Scale bars in pictures from panel D and E represent 50 μm.
(A) Detection of SARS-CoV-2 RNA by in situ hybridization (ISH; brown DAB staining) and (B) its spike protein by immunohistochemistry (red AEC staining) was found in the same region of two serial 1 μm-thick tissue sections of the adrenal gland. Inserts depict the same regions but were captured at lower magnification showing the chosen area of virus positivity (white squares). Scattered expression of either mRNA or protein can be found in the inner parts of the adrenal gland cortex close to the medulla. Scale bars in pictures from panel A and B represent 100 μm (10 μm in the insert image). (C) Ultrastructural examination of a SARS-CoV-2 triple positive (ISH, immunohistochemistry, and RT-qPCR) adrenal tissue showing numerous viral-like particles in liposome (LIP)-rich adrenocortical cells. A scale bar represents 200 nm. A low magnification picture shown in the insert depicts the region of interest indicated by a green arrow in the enlarged picture. Scale bar in insert indicates 1 μm distance. (D) A positive immunofluorescent red signal (CY3) indicating the expression of spike protein in SARS-CoV-2 infected human adrenocortical cells. (E) Lack of positive signal (CY3) in mock-infected control cells. Adrenocortical cells were additionally stained with an antibody against side-chain cleavage enzyme (CYP11A1), which is a steroidogenic marker (green signal; CY5). Nuclei were counterstained with Hoechst 33342 dye (blue signal). Scale bars in pictures from panel D and E represent 50 μm.
The adrenal glands are a popular target amongst invading pathogens, including SARS-CoV.
https://pubmed.ncbi.nlm.nih.gov/15141376/
As a result of SARS-CoV-2 sharing some features and morphology with SARS-CoV, including the ACE2 protein and the transmembrane protease serine subtype 2, direct targeting in COVID-19 infections is possible.
The study team compared the adrenal gland tissues from the 40 deceased patients with the adrenal gland tissues of patients who died before the COVID-19 pandemic to test their theory. In 18 of the 40 cases, the study team used a monoclonal antibody to confirm the SARS-CoV-2 spike protein in adrenocortical cells.
Significantly, the study findings showed detectable evidence of SARS-CoV-2 spike protein in the adrenal cortex. SARS-CoV-2 expression was observed in 15 out of 30 adrenal gland tissues of patients who died from COVID-19 illness.
It should be noted however, a technical limitation of the study was that the concordance rate of all detection tools including, in situ hybridization, immunohistochemistry, and quantitative reverse transcription PCR, was at 23%. This may be due to a low number of virus-positive cells remaining in the tissue.
A detailed ultrastructural analysis of adrenal tissue using all three detection tools was used for a triple-positive patient case.
Study findings showed an abundance of SARS-CoV-2 virus-like particles in cells with high amounts of liposomes-a characteristic of adrenocortical cells.
Further in-vitro experiments confirmed that adrenocortical cells are vulnerable to SARS-CoV-2 infection through detection of an uptake of the spike protein and other viral particles in adrenocortical cells.
The study team also looked for signs of cell necrosis induced in sepsis-mediated adrenal gland damage. Necrosis in adrenal glands involves the loss of membrane integrity and molecular patterns that promote tissue inflammation.
The study findings showed that necroptosis is likely not involved in COVID-19-associated damage to the adrenal medulla.
It should be noted however that in deceased COVID-19 patients, there was increased expression of a protein known as phospho Mixed Lineage Kinase Domain Like Pseudokinase (pMLKL) involved in necroptosis activation. pMLKL expression is also seen in the adrenal glands of patients who died before the pandemic. However, in the adrenal cortex, pMLKL expression was seen in virus-positive regions of the adrenal cortex, suggesting SARS-CoV-2 infection directly triggered necroptosis in infected cells only in the adrenal cortex.
Corresponding author Dr Stefan R Bornstein from the Department of Internal Medicine III, Technische Universität Dresden told Thailand
Medical News, “In summary, in our study of 40 patients who died from COVID-19, we did not observe widespread degradation of human adrenals that might lead to manifestation of the adrenal crisis. However, our study shows that the adrenal gland is a prominent target for the viral infection and ensuing cellular damage, which could trigger a predisposition for adrenal dysfunction. Whether those changes directly contribute to adrenal insufficiency seen in some patients with COVID-19 or lead to its complications (such as long COVID) remains unclear. Large multicentre clinical studies should address this question.”
For the latest
COVID-19 Research, keep on logging to Thailand Medical News