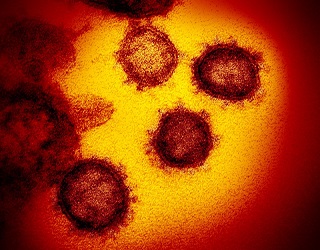
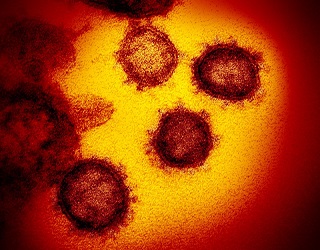
BREAKING! Japanese Study Uncovers That SARS-CoV-2 Impairs The Insulin Growth Factor (IGF) Signaling Pathway With Detrimental Health Implications!
Source: Medical News -SARS-CoV-2 Research Jul 07, 2022 2 years, 9 months, 2 weeks, 5 days, 4 hours, 16 minutes ago
A new study by researchers from Osaka University-Japan has uncovered that SARS-CoV-2 infections impairs the human host’s IGF or Insulin Growth Factor signaling pathway. This can result in a variety of metabolic health conditions as well as numerous detrimental health effects which can also contribute to the conditions of Long COVID.
The insulin-like growth factor-1 receptor (IGF-1R) signaling pathway is a complex and tightly regulated network which is critical for cell proliferation, growth, and survival. IGF-1R is a potential therapeutic target for patients with many different malignancies and its impairment can lead to various health conditions besides different types of metabolic and endocrine issues including organs like heart and kidney damage and also various cancers!
https://www.sciencedirect.com/science/article/pii/S2352304214000373
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4164051/
https://pubmed.ncbi.nlm.nih.gov/30735831/
https://link.springer.com/article/10.1007/s00125-020-05190-9
https://pubmed.ncbi.nlm.nih.gov/25151409/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4715090/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6323188/
https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-015-0762-z
It has already been known that COVID-19 can cause multiple organ damages as well as metabolic abnormalities such as hyperglycemia, insulin resistance, and new onset of diabetes.
The insulin/IGF signaling pathway plays an important role in regulating energy metabolism and cell survival, but little is known about the impact of SARS-CoV-2 infection.
The study team aimed to investigate whether SARS-CoV-2 infection impairs the insulin/IGF signaling pathway in the host cell/tissue, and if so, the potential mechanism and association with COVID-19 pathology.
In order to determine the impact of SARS-CoV-2 on insulin/IGF signaling pathway, the study team used transcriptome datasets of SARS-CoV-2 infected cells and tissues from public repositories for a wide range of high-throughput gene expression data: autopsy lungs from COVID-19 patients compared to the control from non-COVID-19 patients; lungs from a human ACE2 transgenic mouse infected with SARS-CoV-2 compared to the control infected with mock; human pluripotent stem cell (hPSC)-derived liver organoids infected with SARS-CoV-2; adipose tissues from a mouse model of COVID-19 overexpressing human ACE2 via adeno-associated virus serotype 9 (AAV9) compared to the control GFP after SARS-CoV-2 infection; iPS-derived human pancreatic cells infected with SARS-Co
V-2 compared to the mock control. Gain and loss of IRF1 function models were established in HEK293T and/or Calu3 cells to evaluate the impact on insulin signaling. To understand the mechanistic regulation and relevance with COVID-19 risk factors, such as older age, male sex, obesity, and diabetes, several transcriptomes of human respiratory, metabolic, and endocrine cells and tissue were analyzed.
To estimate the association with COVID-19 severity, whole blood transcriptomes of critical patients with COVID-19 compared to those of hospitalized noncritical patients with COVID-19.
Shockingly, the study findings showed that SARS-CoV-2 infection impaired insulin/IGF signaling pathway genes, such as IRS, PI3K, AKT, mTOR, and MAPK, in the host lung, liver, adipose tissue, and pancreatic cells. The impairments were attributed to interferon regulatory factor 1 (IRF1), and its gene expression was highly relevant to risk factors for severe COVID-19; increased with aging in the lung, specifically in men; augmented by obese and diabetic conditions in liver, adipose tissue, and pancreatic islets.
It was also found that IRF1 activation was significantly associated with the impaired insulin signaling in human cells.
IRF1 intron variant rs17622656-A, which was previously reported to be associated with COVID-19 prevalence, increased the IRF1 gene expression in human tissue and was frequently found in American and European population. This could also help explain why Westerners are more badly affected by SARS-CoV-2 infections.
It was also discovered that critical patients with COVID-19 exhibited higher IRF1 and lower insulin/IGF signaling pathway genes in the whole blood compared to hospitalized noncritical patients. Hormonal interventions, such as dihydrotestosterone and dexamethasone, ameliorated the pathological traits in SARS-CoV-2 infectable cells and tissues.
The study findings provide the first scientific evidence that SARS-CoV-2 infection impairs the insulin/IGF signaling pathway in respiratory, metabolic, and endocrine cells and tissues. This feature likely contributes to COVID-19 severity with cell/tissue damage and metabolic abnormalities, which may be exacerbated in older, male, obese, or diabetic patients.
The study findings were published in the peer reviewed journal: Metabolism.
https://www.metabolismjournal.com/article/S0026-0495(22)00114-7/fulltext#
The current COVID-19 pandemic, caused by the rapid outbreak of the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), has significantly affected the global healthcare system and economy. Numerous studies have reported that individuals of older age, as well as those with certain comorbidities like obesity and diabetes, are at a higher risk of contracting severe SARS-CoV-2 infection.
Despite the fact that Although most COVID-19 patients suffer mild to moderate symptoms, 10-15% develop severe pneumonia-like symptoms. In some individuals, COVID-19 causes tissue damage and triggers metabolic abnormalities, which can include the abnormal synthesis of lipids, insulin, and amino acids. The underlying molecular mechanism associated with these metabolic anomalies has yet to be determined.
Many past studies have revealed that the insulin/insulin-like growth factor 1 (IGF) signaling pathway has an important role in energy metabolism. Other molecular pathways associated with energy uptake and utilization are the downstream AKT/mTOR/MAPK pathway and ligand/receptor interactions that initiate cellular signaling through IRS/PI3K.
It has been known that insulin resistance or abnormal insulin/IGF responses occurs due to impairment in the insulin/IGF signaling pathway in organs and tissues. In addition to insulin resistance, an impaired insulin/IGF signaling pathway also leads to hyperglycemia, diabetes, hyperlipidemia, and obesity.
Importantly past studies have showed that the systemic knockout of the insulin receptor in mice initiated an early onset of diabetes. Additionally, some mice died due to ketoacidosis.
https://www.nature.com/articles/ng0196-106
https://www.proquest.com/openview/748e9729e16bd3ab01b5e853511cdc2e/1?pq-origsite=gscholar&cbl=24890
.jpg) Graphical Abstract
Graphical Abstract
The inhibition of the insulin/IGF signaling pathway in adipose tissue results in the loss of adipose tissue. This condition also causes severe metabolic syndrome, thus demonstrating that insulin/IGF signaling is vital for the functioning of pancreatic beta cells.
https://diabetesjournals.org/diabetes/article/65/8/2187/35172/Lipodystrophy-Due-to-Adipose-Tissue-Specific
Past studies have also demonstrated that knockout of the insulin receptor in beta cells caused a reduction in insulin production, a condition otherwise known as diabetes mellitus.
https://www.sciencedirect.com/science/article/pii/S0092867400805462
It should also be noted that the association between insulin resistance and lung dysfunction in humans has also been documented in the literature.
https://www.sciencedirect.com/science/article/abs/pii/S126236360800164X
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1464-5491.2010.03073.x
https://diabetesjournals.org/care/article/26/6/1915/26299/Lung-Dysfunction-in-Diabetes
https://www.sciencedirect.com/science/article/abs/pii/S0091674915000998
However, to date, very few studies have determined the impact of SARS-CoV-2 infection on the insulin/IGF signaling pathway.
The study team aimed toevaluate the impact of SARS-CoV-2 on the insulin/IGF signaling pathway.
The study team obtained high-throughput transcriptome data related to SARS-CoV-2 infected cells and tissues from public databases.
The study team also obtained autopsy data on the lungs of both COVID-19 and non-COVID-19 control patients. They further assessed the impact of SARS-CoV-2 infection on human pluripotent stem cell (hPSC)-derived liver organoids.
The study team evaluated the impact of IRF1 on insulin signaling using HEK293T and Calu3 cells. To evaluate the role of COVID-19 risk factors such as sex, age, obesity, and diabetes on mechanistic regulation, the scientists analyzed several transcriptomes of human metabolic, respiratory, and endocrine cells and tissues.
Interestingly, a strong correlation between an impaired insulin/IGF signaling pathway and severe COVID-19 was observed.
Furthermore, the study team also found that SARS-CoV-2 infection affects a wide range of insulin/IGF signaling pathways in the lungs, liver, pancreatic cells, and adipose tissue.
The IRF1 receptors were also found to be associated with the impairment of the insulin/IGF signaling pathway. Past studies have linked the expression of IRF1 with male sex, older age, diabetes, and COVID-19. In fact, a higher expression of IRF1 has been associated with obesity, older age, diabetes, and/or genetic variant, which might be intensified due to the upregulation of IRF1 in response to SARS-CoV-2 infection.
Many research studies have also shown that IRF1 intron variant rs17622656-A is abundantly present in European and American populations.
The study findings report that COVID-19 pathology is governed by the higher expression of IRF1 and lower expression of insulin/IGF signaling pathway molecules.
Interestingly, hormonal treatment in the form of dihydrotestosterone and dexamethasone has effectively reduced the gene expression of IRF1.
These existing findings led the study team to hypothesize that this treatment could increase the insulin/IGF signaling pathway in SARS-CoV-2 infected cells and tissues and, as a result, improve cellular signaling.
The research findings strongly indicate that SARS-CoV-2 infection not only affects respiratory tracts but also impairs endocrine and metabolic cells and tissues. Identifying the molecular basis of these pathological observations could therefore aid in the development of future COVID-19 therapeutics.
Importantly impairment of the insulin/IGF signaling pathway in cells and tissues of the liver, lungs, and pancreas leads to the development of multiorgan dysfunction. Since COVID-19 causes impairment of the insulin/IGF signaling pathway, it is also associated with the downregulation of various metabolic pathways including the citrate cycle, lipid metabolism, beta-oxidation, amino acid metabolism, and carbohydrate metabolism, and respiratory electron transport.
The study team also emphasized the potential for COVID-19-mediated inflammation to induce insulin resistance in various cells and tissues.
The research findings showed that dihydrotestosterone and dexamethasone treatments could ameliorate insulin resistance and metabolic abnormalities in COVID-19 patients.
The study team says that in the future, more physiological, pathological, and pharmacological experiments must be conducted to estimate the clinical efficacy of this treatment in COVID-19 patients.
Thailand
Medical News would further like to add that the impairment of this pathway adds to the list of 283 of the 347 already known cellular pathways and various genes that are either disrupted, damaged or made dysfunctional by the SARS-CoV-2 coronavirus and its various viral proteins, that can cause serious long term health issues and which will aid in shortening the lifespan of all those exposed to the SARS-CoV-2 virus. We postulate on an optimistic perspective that a majority of the exposed population will only have between 5 to 8 years left or shorter if they are exposed to reinfections!
https://www.thailandmedical.news/news/breaking-hypothesis-that-majority-exposed-to-sars-cov-2-will-have-shortened-lifespans-validated-by-study-showing-nsp2-impairs-human-4ehp-gigyf2-comple
For the latest
SARS-CoV-2 Research, keep on logging to Thailand
Medical News.
.jpg)