BREAKING NEWS! Doctors Warns That SARS-CoV-2 Infections Can Cause Pancytopenia. Increasing incidences Sparks Concerns!
COVID-19 News - SARS-CoV-2 Infections - Pancytopenia Jul 24, 2023 2 years, 4 months, 2 weeks, 6 days, 22 hours, 2 minutes ago
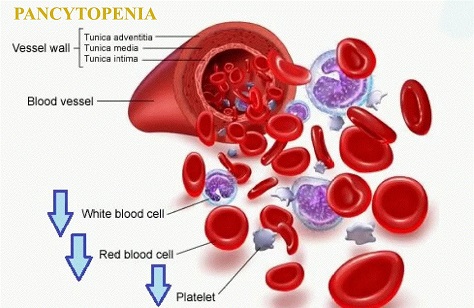
Pancytopenia occurs when an individual's blood shows unusually reduced levels of all three types of blood cells - red blood cells, white blood cells, and platelets.
COVID-19 News: In the ongoing battle against the COVID-19 pandemic, medical experts have recently issued a warning regarding a rare but concerning complication associated with the SARS-CoV-2 virus. This complication, known as Pancytopenia, has been observed in some individuals who have contracted COVID-19, leading to a triage of low blood cell counts, including anemia, leukopenia, and thrombocytopenia. While it is crucial to understand that Pancytopenia itself is not a disease, but rather a symptom of an underlying condition, its presence in COVID-19 patients has sparked growing concerns within the medical community.
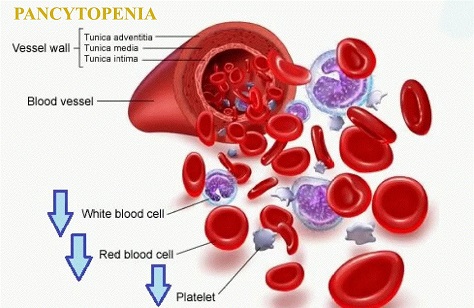
Pancytopenia manifests when a person's blood contains abnormally low levels of all three types of blood cells - red blood cells, white blood cells, and platelets. This condition can be triggered by various factors, including nutritional deficiencies, medications, autoimmune diseases, malignancies, and infections. Among the infectious causes, certain viruses such as human immunodeficiency virus (HIV), cytomegalovirus (CMV), Epstein-Barr virus (EBV), and parvovirus B19 have been associated with Pancytopenia. However, it is essential to note that Pancytopenia has not been commonly observed in patients with COVID-19 disease, making it a relatively rare complication till the debut of the Omicron variant!
The symptoms of Pancytopenia can vary, depending on the type and severity of blood cell deficiency. Patients may experience symptoms associated with anemia, such as headaches, cold hands and feet, fatigue, weakness, pale or yellowish skin, shortness of breath, irregular heartbeat, chest pain, dizziness, and lightheadedness. Leukopenia, which is a reduced white blood cell count, may lead to symptoms such as infections, chills, fever, and sweating. Thrombocytopenia, the condition of low platelet count, can cause symptoms like easy or excessive bruising, prolonged bleeding from cuts, fatigue, enlarged spleen, nosebleeds, bleeding from the gums, blood in urine or stools, and heavy menstrual flow.
While some of these symptoms may not be alarming, certain serious symptoms require immediate medical attention, including loss of consciousness, confusion, fever over 38.4 degrees Celsius, heavy bleeding, seizures, convulsions, and extreme shortness of breath.
Medical professionals have noticed a connection between viral infections and hematologic dysfunction for a long time as reported in various past studies and also
COVID-19 News reports. With the rapid spread of COVID-19, numerous hematologic manifestations have emerged, leading to a better understanding of the virus's impact on blood cells. While there have been several reports of immune thrombocytopenic purpura in COVID-19 patients, the occurrence of concurrent lymphopenia and anemia has been relatively sparse.
However, recent cases have highlighted the emergence of COVID-induced Pancytopenia, which has been observed months after the initial COVID infection and sometimes persists despite initial treatment with in
travenous immunoglobulin (IVIG) and steroids.
https://www.mdpi.com/1648-9144/59/7/1349
https://www.elsevier.es/en-revista-medicina-clinica-english-edition--462-avance-resumen-pancytopenia-during-sars-cov-2-infection-S2387020620304551
https://www.ajtmh.org/view/journals/tpmd/107/1/article-p162.xml
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8743232/
https://www.longdom.org/open-access/an-atypical-case-of-sarscov-2induced-pancytopenia-88911.html
https://www.researchsquare.com/article/rs-657352/v1
https://www.hindawi.com/journals/crihem/2022/8739295/
https://www.cureus.com/articles/129220-covid-19-and-subsequent-development-of-pancytopenia-with-concurrent-disseminated-intravascular-coagulation#!/
https://www.sciencedirect.com/science/article/pii/S2152265021000069
https://amjcaserep.com/abstract/full/idArt/937500
https://onlinelibrary.wiley.com/doi/10.1002/jmv.26566
https://www.mdpi.com/1648-9144/58/9/1282
https://academic.oup.com/ofid/article/8/2/ofab017/6103190
https://www.editorialmanager.in/index.php/ijofb/article/view/730
https://jcimcr.org/pdfs/JCIMCR-v3-2008.pdf
The exact mechanisms by which SARS-CoV-2 induces Pancytopenia are not entirely clear, but various hypotheses have been proposed by experts. One such hypothesis suggests that the virus causes myelosuppression by triggering an autoimmune response, leading to the destruction of blood cells. SARS-CoV-2 primarily targets angiotensin-converting enzyme 2 receptors, which have also been found in bone marrow. The binding of the virus to these receptors may lead to downstream effects, including Pancytopenia. Additionally, there have been case reports suggesting that the proinflammatory cytokines produced during the infection might impair hematopoiesis. The virus may also directly affect hematopoietic progenitor cells in the lungs, leading to a reduction in blood cell production.
Despite the concerns surrounding COVID-induced Pancytopenia, medical experts emphasize that the condition is typically self-limiting and may resolve with supportive care and addressing any underlying risk factors. Some patients have shown improvement with supportive care alone, and follow-up assessments have indicated a return to normal blood cell function.
As the medical community continues to learn more about the complexities of COVID-19 and its potential complications, it is crucial for healthcare professionals to remain vigilant. When encountering patients with recent COVID-19 infections who present with a decrease in all three blood cell lines, it is essential to consider Pancytopenia as a possible cause. While further investigations may be necessary, including ruling out other concurrent causes, invasive tests such as bone marrow biopsies may not always be required, especially if the patient shows improvement with supportive care.
In conclusion, the emergence of Pancytopenia as a complication of COVID-19 raises important questions for medical researchers and practitioners. Understanding the mechanisms behind this condition and identifying risk factors that may contribute to its development will be vital in providing effective care and management for COVID-19 patients.
It should also be noted that the current COVID-19 mRNA vaccines can also cause pancytopenia as an adverse effect.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8863340/
https://www.dovepress.com/bone-marrow-suppression-secondary-to-the-covid-19-booster-vaccine-a-ca-peer-reviewed-fulltext-article-JBM
For the latest
COVID-19 News, keep logging to Thailand Medical News.