BREAKING! Oxford Study Warns That Many Breathless Long COVID Patients Have Impaired Gas Transfer In Lungs Which Cannot Be Detected By Normal CT Scans!
Source: Long COVID - Breathless Feb 05, 2022 3 years, 10 months, 2 weeks, 5 days, 16 hours, 34 minutes ago
A new study led by researchers from University of Oxford-UK and Oxford University Hospitals NHS Trust-UK that was also supported by experts from the University of Birmingham-UK, University of Sheffield-UK and GE Healthcare-Germany has found that many non-hospitalized breathless
Long COVID patients have impaired gas transfer in lungs which alarmingly cannot be detected by normal CT scans.
These abnormalities in the lungs can only be detected by a new imaging device by GE company that uses Hyperpolarized Xenon Magnetic Resonance Imaging (Hp-XeMRI) but is not available in many hospitals globally.
Long-COVID is an umbrella term used to describe ongoing symptoms following COVID-19 infection after four weeks. Symptoms are wide-ranging but breathlessness is one of the most common and can persist for months after the initial infection. Investigations including Computed Tomography (CT), and physiological measurements (lung function tests) are usually unremarkable and are unable to detect the abnormalities.
The detailed mechanisms driving breathlessness remain unclear, and this may be hindering the development of effective treatments.
In the study, eleven non-hospitalized Long-COVID (NHLC, 4 male), 12 post-hospitalized COVID-19 (PHC, 10 male) patients were recruited from a Post-COVID Assessment clinic, and thirteen healthy controls (6 female) were recruited to undergo Hyperpolarized Xenon Magnetic Resonance Imaging (Hp-XeMRI).
NHLC and PHC participants underwent contemporaneous CT, Hp-XeMRI, lung function tests, 1-minute sit-to-stand test and breathlessness questionnaires. Statistical analysis included group and pair-wise comparisons between patients and controls, and correlations between patient clinical and imaging data.
All the NHLC and PHC patients were 287 ± 79 [range 190-437] and 149 ± 68 [range 68-269] days from infection, respectively.
The study findings showed that all NHLC patients had normal CT scans, and the PHC had normal or near normal CT scans (0.3/25 ± 0.6 [range 0-2] and 7/25 ± 5 [range 4-8], respectively).
There was a significant difference in TLco (%) between NHLC and PHC patients (76 ± 8 % vs 86 ± 8%, respectively, p = 0.04) but no differences in other measurements of lung function. There were significant differences in RBC:TP mean between volunteers (0.45 ± 0.07, range [0.33-0.55]) and PHC (0.31 ± 0.11, [range 0.16-0.37]) and NHLC (0.35 ± 0.09, [range 0.26-0.58]) patients, but not between NHLC and PHC (p = 0.26).
Importantly Hp-XeMRI results were abnormal in the majority (7/11) of NHLC patients, indicating that pulmonary gas transfer is impaired many months and in some, over a year after their initial infection.
All the NHLC participants in this study with abnormal Hp-XeMRI were imaged more than 6 months after their initial infection, indicating that these abnormalities are not a transient phenomenon following acute infection. The NHLC patients were also on average further from their initial infection than the PHC group (287 v 149 days). Interestingly, the measured abnormality on Hp-XeMRI appears to be only marginally greater in the PHC than the NHLC patients despite those admitted to hospital having had a pres
umed clinically more severe acute infection.
There are RBC:TP abnormalities in NHLC and PHC patients, with NHLC patients also demonstrating lower TLco than PHC patients despite their having normal CT scans. These abnormalities are present many months after the initial infection.
The study findings indicated that hyperpolarized Xenon MRI and TLco demonstrate significantly impaired gas transfer in non-hospitalized long-COVID patients when all other investigations are normal.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.medrxiv.org/content/10.1101/2022.02.01.22269999v1
The COVID-19 disease causes symptoms such as anosmia, coughing, headaches to more deadly results such as organ failure and lung damage.
Most recently, 'long-COVID' has come to the media's attention and has, as a result, gained significant attention. Long-COVID is seen in patients who have suffered from infection with the SARS-CoV-2 virus, recovered enough to test negative for the virus on both PCR and rapid antigen testing, but continue to suffer from symptoms for a significant time after.
There are many possible factors causing long COVID that may be acting solely or collectively including viral persistence, direct ‘attack’ on the organs or tissues by the SARS-CoV-2 virus itself or by its viral proteins, the after effects of cytokine storms or persistent inflammation, the disruption and dysfunction of numerous cellular pathways in the human hos by the virus, the dysregulation of expression of various host genes by the virus and lastly the dismantling and dysregulation of the human immunes responses by the virus.
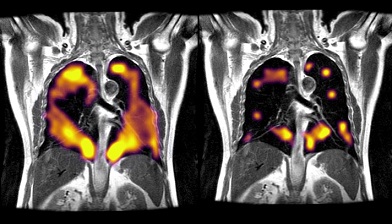
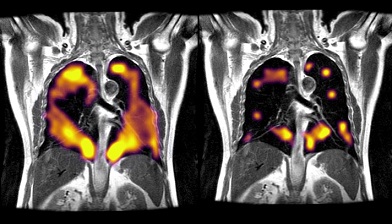
.jpg) Example CT, proton, Gas, TP, and RBC imaging from Long-COVID patients. The top row is a patient with RBC:TP = 0.49, the middle row is a patient with RBC:TP of 0.31, and the bottom row is a patient with RBC:TP = 0.24
Example CT, proton, Gas, TP, and RBC imaging from Long-COVID patients. The top row is a patient with RBC:TP = 0.49, the middle row is a patient with RBC:TP of 0.31, and the bottom row is a patient with RBC:TP = 0.24
Although anosmia is the most reported condition recently, breathlessness and fatigue are also very common, sometimes to the extent that sufferers find it difficult to complete basic tasks such as reaching high shelves and walking short distances.
Scientists have been investigating the symptoms and effect on the lungs in those who suffered from hospitalization due to COVID-19 but fully recovered and non-hospitalized sufferers of long-COVID.
The Oxford led study team recruited study participants from the Oxford Post-COVID Assessment clinic. Patients were eligible for inclusion if they had been previously hospitalized with COVID-19 (PHC), had not been hospitalized but had been diagnosed with Long-COVID (NHLC), or if they were healthy volunteers to act as controls. All participants were required to have no smoking history, lung or airway disease history, and a normal or near-normal computed tomography (CT) scan. COVID-19 diagnosis must have been confirmed using PCR.
The study team performed analysis on each participant cohort independently, assessing the correlation between variables using Spearman's correlation and using a linear fit for significantly correlated variables. After separating data into non-hospitalized long COVID-19 patients and hospitalized COVID-19 patients, the analysis was then repeated for group-dependent associations with clinical symptoms. Non-parametric ANOVA and Tukey post-hoc tests with Bonferroni correction for multiple comparisons helped compare between RBC:TP in patient and volunteer groups.
Altogether a total of 11 NHLC and 12 PHC patients were recruited, alongside 13 health volunteers. The average Hb for NHLC and health controls was 144/145, respectively. Both NHLC and PHC showed breathlessness with an average Dyspnoea-12 score of 9 and 10, and mBORG pre and post sit-stand test of 2 and 7 beforehand, and 2 and 5 afterward.
It was found that the NHLC and PHC participants scored overwhelmingly lower than the healthy controls for the number of repetitions they could do on the sit-stand test.
There were also significant differences in RBC:TP means between healthy volunteers and PHC/ NHLC, as well as between PHC and NHLC, with health volunteers averaging at 0.46 and PHC/NHLC averaging at 0.31/0.35.
Also, there was no significant difference in Forced Expiratory Volume between groups, but NHLC showed lower mean gas transfer than PHC participants. NHLC participants showed a significant correlation between TLco (%) and RBC:TP means and standard deviation.
The study team however showed that the Hp-X eMRI results were abnormal in most long-COVID patients, indicating that gas transfer could be impaired over a year after the initial infection.
The Hp-X eMRI scans also showed that the abnormalities detected in both PHC and NHLC patients were very similar. The abnormalities also lasted at least six months for NHLC patients. Unfortunately, the testing did not reveal the relationship between the abnormalities detected on the scan and the breathlessness typically seen in NHLC patients.
The study team did however theorize that infection with SARS-CoV-2 induces damage to the microstructures in either the blood or alveolar membrane volume, reducing diffusion capacity.
Another possibility is that the direct damage to the lungs due to either the virus or inflammatory sequelae could be the cause which was supported by detecting a faint 'footprint' of COVID-19 pneumonia.
The study team concluded that they have successfully identified impairment in the gas transfer in lungs of long-COVID patients who are experiencing breathlessness, which provides preliminary evidence that lung abnormalities that cannot be detected through typical imaging cause some symptoms.
Although the underlying pathophysiology is unknown, researchers have expanded their study to a larger cohort of patients, including long-COVID patients not suffering from breathlessness. They hope to understand the condition in the future better.
Thailand
Medical News would like to add that we have successfully formulated a new phytochemical based therapeutic product to help long COVID-19 patients with the healing and repair of their lungs and the regeneration of epithelial cells and tissues and the compound that has already passed safety tests will shortly be undergoing a large observation clinical trial study. Those interested to be part of the study can contact us. (Only in the United States, Canada, Australia, New Zealand, Singapore, Japan, All Over Europe Except UK and Sweden.)
For more on
Long COVID, keep on logging to Thailand Medical News.
.jpg)