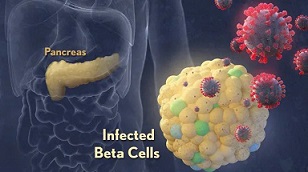
BREAKING! SARS-CoV-2 Directly Infects The Pancreatic Islets And Causes Pancreatic Inflammation That Can Lead To Post COVID Hyperglycemia And Other Issues!
Source: Medical News - SARS-CoV-2 - Pancreas May 05, 2022 2 years, 11 months, 3 weeks, 11 hours, 3 minutes ago
Italian researchers from Universitá di Milano, have in a new study found that the SARS-CoV-2 coronavirus is able to directly and also indirectly affect the pancreatic islets of the host and cause pancreatic inflammation that can lead to Post COVID Hyperglycemia and other health conditions and issues!
It is interesting that ever since the Omicron wave, incidences of not only hyperglycemia in previously healthy individuals have exponentially gone up Post COVID individuals, but Thailand
Medical News has also been observing a rise in occurrences of acute and chronic pancreatitis globally!
Numerous studies have already shown that SARS-CoV-2 infection may induce metabolic distress, leading to hyperglycemia in patients affected by COVID-19.
The study team investigated the potential indirect and direct effects of SARS-CoV-2 on human pancreatic islets in 10 patients who became hyperglycemic after COVID-19.
Although there was no evidence of peripheral anti-islet autoimmunity, the serum of these patients displayed toxicity on human pancreatic islets, which can be abrogated by the use of anti-IL1β, anti-IL-6 and anti-TNF-α, cytokines known to be highly upregulated during COVID-19.
Importantly, the study findings showed that the receptors of those aforementioned cytokines were highly expressed on human pancreatic islets. An increase in peripheral unmethylated INS DNA, a marker of cell death, was evident in several patients with COVID-19.
Furthermore, pathology of the pancreas from deceased hyperglycemic patients who had COVID-19, revealed mild lymphocytic infiltration of pancreatic islets and pancreatic lymph nodes.
Also of significance, SARS-CoV-2-specific viral RNA, along with the presence of several immature insulin granules or proinsulin, were detected in post-mortem pancreatic tissues, suggestive of β-cell altered proinsulin processing, as well as β-cell degeneration and hyperstimulation.
The study findings reveal that SARS-CoV-2 negatively affects human pancreatic islets function and survival by creating inflammatory conditions and possibly with a direct tropism, which may in turn lead to metabolic abnormalities observed in patients with COVID-19 and also other pancreatic conditions.
The study findings were published in the peer reviewed journal: Diabetes.
https://diabetesjournals.org/diabetes/article/doi/10.2337/db21-0926/146863/Indirect-and-Direct-Effects-of-SARS-CoV-2-on-Human
It should be noted that already in the past, the correlation between new-onset hyperglycemia diagnosis with COVID-19 infection has been widely reported.
This is primarily due to the higher number of hyperglycemic incidents during COVID-19 infections as compared to those during SARS-CoV-1 or hepatitis C infections.
The study team examined the direct and indirect effects of SARS-CoV-2 infection on human pancreatic islets in COVID-19 patients having new-onset hyperglycemia.
The researchers collected serum samples from 10 patients who were hospitalized d
ue to COVID-19 and who were subsequently diagnosed with new-onset hyperglycemia.
Also, serum samples were obtained from another 10 patients who reported COVID-19 recovery.
Importantly, all eligible study participants were COVID-19 positive and had no history of diabetes before hospital admission. The study team also collected serum samples from healthy control individuals.
For the study, levels of insulin, glutamic acid decarboxylase (GAD), islet antigen 2 (IA-2), and zinc transporter eight autoantibodies (ZnT8A) were estimated using a fully validated enzyme-linked immunosorbent assay (ELISA).
Also, human pancreatic islets were cultivated with/without interleukin-1 beta (IL-1β), IL-13, IL-6, tumor necrosis factor-alpha (TNFα), and inducible protein 10 (IP-10).
The study team also assessed the apoptosis and function of human pancreatic islets via ELISA 24 hours after incubation.
The study team nest cultured the human pancreatic islets were and exposed it to recombinant human IL-1β, recombinant human TNFα, recombinant human IL-13, recombinant human IL-6, recombinant human IP-10, or serum samples from patients infected with acute COVID-19 or from COVID-19-recovered patients.
The research team also performed immunoneutralization studies along with ribonucleic acid (RNA) extraction from pancreatic islets collected from healthy donors.
Detailed gene expression analysis was also conducted, and the resulting transcripts were normalized to evaluate the relative abundance of the transcripts.
The study team also obtained pancreatic tissues from deceased COVID-19 patients, deceased controls, or deceased individuals with type 2 diabetes.
β-cell death was detected by examining unmethylated insulin deoxyribonucleic acid (DNA) derived from β-cell. Total RNA was obtained from post-mortem pancreatic tissues of COVID-19-infected hyperglycemic patients. The SARS-CoV-2 expression in these tissues was estimated by detecting SARS-CoV-2-specific RNA using real-time reverse transcription-polymerase chain reaction (rtRT-PCR).
The research findings showed that COVID-19-infected and COVID-19-recovered patients tested negative for anti-islet autoantibodies, despite substantial dysregulation of the glycometabolic control.
Also, a significant reduction in the ratios of unmethylated (U) to methylated (M) INS DNA was observed in COVID-19-infected patients but not in recovered patients.
Alarmingly however, a significant rise was found in the number of copies of U and M INS DNA in infected patients as opposed to recovered patients in comparison to the control subjects. This indicated widespread destruction of pancreatic tissue in COVID-19-infected patients.
The study team also found that apoptosis of human pancreatic islets was associated with a severe reduction in insulin secretion in cohorts including patients who were infected and recovered from COVID-19.
Interestingly, when human pancreatic islets were exposed to sera collected from type 2 diabetes patients, a slight reduction in insulin secretion was observed along with a higher increase in the number of human pancreatic islet deaths.
It was also noted that receptome analysis showed that human pancreatic islets expressed several cytokine receptors that bind to cytokines which were upregulated in the secretome of COVID-19-infected patients. In particular, the receptors for IL-1β, IL-6, IL-13, and TNFα were expressed by human pancreatic islets. The study also confirmed an increase in the impact of single and combined cytokines mediated by apoptosis in serum samples of COVID-19 patients. IL-1β, IL-6, IP-10, IL-13, and TNFα also induced the apoptosis of the human pancreatic islets. The study team also observed a reduction in insulin secretion with each cytokine or combination of these five cytokines.
Also of significance, the immunoneutralization assay showed a decline in apoptosis mediated by human pancreatic islet apoptosis in the serum samples after adding blocking or neutralizing antibodies anti-IL-1 and anti-IL-6 to the serum assay.
Simultaneous immunoneutralization of IL-1, IL-6, and IL-13 also prevented the apoptosis of the pancreatic islets, which further reversed the levels of apoptotic human pancreatic islets to that of baseline levels.
The research findings showed that new-onset hyperglycemia in COVID-19-infected patients may be due to the pro-inflammatory activities induced by the release of cytokines in pancreatic cells during a SARS-CoV-2 infection.
Post COVID patients need to also keep on a constant look out for symptoms associated by both hyperglycemia and also pancreatitis and also get frequent health screenings.
For more on
SARS-CoV-2 and the Pancreas, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/coronavirus-news-cedars-sinai-medical-center-study-confirms-that-the-sars-cov-2-virus-infects-the-pancreas-directly
https://www.thailandmedical.news/news/acute-pancreatitis-warning-that-acute-pancreatitis-is-now-manifesting-in-covid-19-patients,-a-condition-never-seen-in-early-stages-of-the-pandemic