BREAKING! SARS-CoV-2 Spike Proteins Bind To Brain’s MAO Enzymes Causing Neurological Issues! Binding Affinity Is Enhanced In Some Emerging Variants!
Source: NeuroCOVID Sep 06, 2021 3 years, 7 months, 2 weeks, 5 days, 22 hours, 57 minutes ago
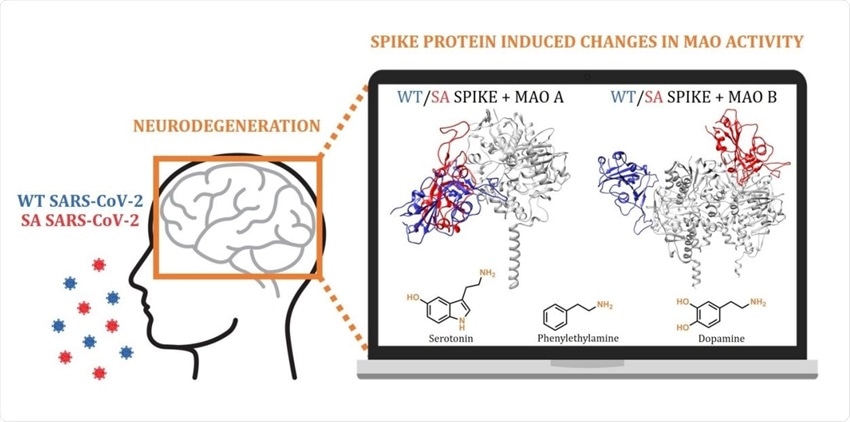
NeuroCOVID: New alarming study findings by researchers from the Ruđer Bošković Institute-Croatia, University of Zagreb-Croatia and the National Institute of Chemistry- have shown that the Spike proteins of the SARS-CoV-2 coronavirus have a strong biding affinity for the enzyme found in the brain called monoamine oxidases (MAO) enzymes and it is as a result of these binding and subsequent disruption in the various neurotransmitters activities and chemical pathways that a various of neurological conditions emerge including neurodegenerative conditions that can result in Parkinson’s or Alzheimer’s disease! Even more worrisome was the fact that the study found that certain emerging variants such as the South African Beta variant because of the Spike mutations, have an even greater enhanced affinity of binding to these monoamine oxidases (MAO) enzymes.
.jpg)
Several lines of evidence indicate that monoamine oxidase (MAO) activity can regulate levels of biogenic amines and neuronal activity in the nervous system. Monoamine oxidase is involved in removing the neurotransmitters norepinephrine, serotonin and dopamine from the brain.
Various past studies have already demonstrated that the SARS-CoV-2 coronavirus and its viral proteins can affect the brain and various neurological aspects either directly or indirectly.
Many published research agrees that COVID-19 is likely to have long-term mental health effects on infected individuals, which signifies a need to understand the role of the virus in the pathophysiology of brain disorders that is currently unknown and widely debated.
The study team’s docking and molecular dynamic simulations show that the affinity of the spike protein from the wild type (WT) and the South African B.1.351 (SA) variant towards the MAO enzymes is comparable to that for its ACE2 receptor. This allows for the WT/SA…MAO complex formation, which changes MAO affinities for their neurotransmitter substrates, thus consequently impacting the rates of their metabolic conversion and misbalancing their levels.
By understanding that this fine regulation is strongly linked with the etiology of various brain pathologies, these study findings are the first to highlight the possibility that the interference with the brain MAO catalytic activity is responsible for the increased neurodegenerative illnesses following a COVID-19 infection, thus placing a neurobiological link between these two conditions in the spotlight.
Alarmingly since the obtained insight suggests that a more contagious SA variant causes even larger disturbances, and with new and more problematic strains likely emerging in the near future, the study team firmly advises that the presented prospect of the SARS-CoV-2 induced neurological complications should not be ignored, but rather requires further clinical investigations to achieve an early diagnosis and timely therapeutic interventions.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.biorxiv.org/content/10.1101/2021.08.30.458208v1
Past studies have suggested that the SARS-CoV-2 coronavirus affects the brain and causes enduring neurological problems. However, how the virus causes various neurological complications and long
-term mental health problems remains under investigation.
This
NeuroCOVID study findings show that the SARS-CoV-2 spike protein has an affinity towards monoamine oxidases (MAO) enzymes. Changes in MAO levels have been the culprit for several neuropsychiatric disorders such as Parkinson’s or Alzheimer’s disease.
Corresponding author, Dr Robert Vianello from the Laboratory for the Computational Design and Synthesis of Functional Materials, Division of Organic Chemistry and Biochemistry, Ruđer Bošković Institute told Thailand Medical News, “Our study findings aid in identifying the critical role of the MAO enzymes towards an increased incidence of neurological disorders in the SARS‐CoV‐2 infected individuals, therefore placing a neurobiological link between these two conditions in the spotlight.”
As a result of the Spike protein binding affinity for the MAO enzymes, it was found that the resulting SARS-CoV-2–MAO complex formation significantly reduced brain MAO activity by lowering MAO affinity toward neurotransmitters.
The study team suggests that based on the findings, the complex could increase the risk of developing a neurodegenerative illness in individuals infected with COVID-19.
The study team created a computer model to evaluate spike protein-ACE2 binding and docking features. Then, they narrowed their focus to the Beta variant with a high ACE2 binding affinity and increased infectivity.A decomposition of the binding affinity revealed several spike protein residues playing a major role in ACE2 binding.
It was found that about 15 spike protein residues belonged to the receptor-binding motif of the receptor-binding domain. They comprised 78% of the total binding energy. The only exception was Lys417 which instead forms a salt bridge with Asp30 from ACE2.
Interestingly the most dominant residue is Tyr501, a mutation of Asn501 in the original SARS-CoV-2 strain. This residue makes up 17% of binding energy.
Alarmingly, the N501Y mutation in the Beta variant helps to increase and enhances the residue’s binding affinity.
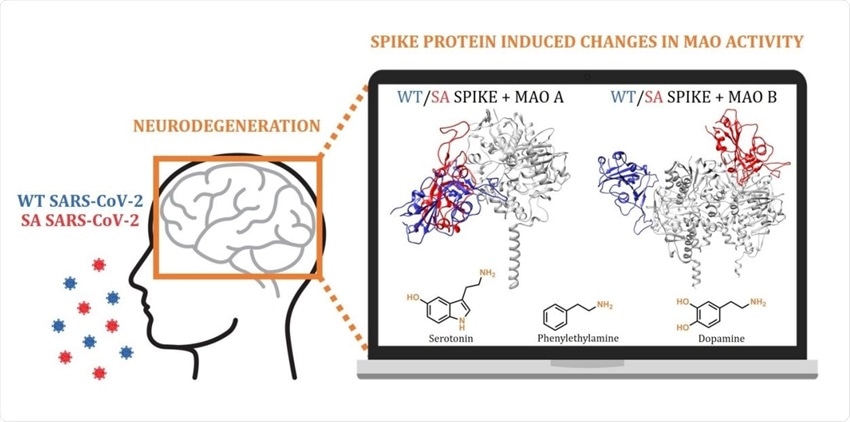 Computational docking and molecular dynamic simulations highlight the possibility that the interference with the brain monoamine oxidase (MAO) catalytic activity is responsible for the increased neurodegenerative illnesses following a COVID‐19 infection.
Computational docking and molecular dynamic simulations highlight the possibility that the interference with the brain monoamine oxidase (MAO) catalytic activity is responsible for the increased neurodegenerative illnesses following a COVID‐19 infection.
However the spike protein residues that do not favor binding include Asp405 and Glu406. These residues are not located in the receptor-binding motif of the receptor-binding domain.
The study findings confirm the original SARS-CoV-2 strain and Beta variant are similar in recognizing ACE2. It also showed that the order of residues contributing to binding remains unchanged, suggesting the spike protein mutations in the Beta variant are responsible for approximately 70% of the overall binding affinity.
The study team used the validating computation set up to investigate potential interactions between the SARS-CoV-2 strains and MAO enzymes. Results showed SARS-CoV-2 links with MAO enzymes through spike protein residues in the receptor-binding motif residue. In addition, the binding affinity towards MAO enzymes increases in more infectious variants.
Surprisingly it was found that in the Beta variant, all three of its spike protein mutations promote MAO-A binding. The mutated Asn417 residue appears to contribute the most to the binding of MAO-A, which could indicate the formation of a SARS-CoV-2 beta variant–MAO-A complex.
Furthermore two spike protein residues in the Beta variant, S-Leu455 and the mutated Asn417, use their backbone carbonyl and side-chain amide atoms to engage with MAO A’s Arg297 residue.
The study findings confirmed that the Beta variant has a higher binding affinity with MAO B than with the ACE2 receptor. A possible reason for the high affinity is the location of different MAO B areas subunits. The researchers suggest the favorable binding between the two could influence the progression of neurological conditions.
Importantly it should be noted that high binding affinity towards MAO negatively impacts MAO interactions with brain amines.
The binding affinity between MAO isoforms and the original SARS-CoV-2 strain affects its interaction with phenylethylamine, serotonin, and dopamine.
The SARS0CoV-2 virus’s impact on MAO’s binding to other substrates is affected even further with the Beta variant. The Beta variant increases MAO affinity towards its substrates and induces higher rates of metabolic degradation, resulting in their depletion.
Dr Vianello warned, “Since the obtained insight suggests that a more contagious Beta variant causes even larger disturbances, and with new and more problematic strains likely emerging in the near future, we firmly advise that the presented prospect of the SARS-CoV-2 induced neurological complications should not be ignored, but rather requires further clinical investigations to achieve an early diagnosis and timely therapeutic interventions.”
Further detailed studies are also underway to analyze the binding affinities and also neurotransmitter disruptions with regards to the spike proteins of the other emerging variants of concern (VOCs) and variants of interests (VOIs).
Importantly, the study findings also prove a point that Thailand Medical News has always been mentioning, various variants have different pathogenesis and affects the various host cellular pathways differently resulting in different clinical manifestations. COVID-19 is not a homogenous disease! Treatment should involve a personalized precision medicine approach.
For more about
NeuroCOVID, keep on logging to Thailand Medical News.
.jpg)