BREAKING! Study Alarmingly Reveals That SARS-CoV-2 Infections Causes Widespread Prevalence Of Inflammatory Microvasculopathy In Brains Of Infected!
Source: Medical News - SARS-CoV-2-Brains May 10, 2022 2 years, 11 months, 2 weeks, 1 day, 22 hours, 22 minutes ago
A new autopsy study involving the brains of 36 deceased COVID-19 patients by researchers from Louisiana State University Health Sciences Center-USA, Southeast Louisiana Veterans Healthcare System-USA and Marshfield Clinic Health System-USA has alarmingly found that SARS-CoV-2 infections causes reactive and acute inflammatory CNS microvasculopathy in the brains of those infected!
The study findings have a huge bearing on long term healthcare and long COVID-19 as more and more studies are emerging that besides affecting the other organs and tissues in the human host, the brain and the CNS system is also being affected by the novel coronavirus directly and indirectly in a number of ways.
To date, hypercytokinemia, the renin-angiotensin system (RAS), and hypoxia have been implicated in brain morbidity in COVID-19.
There is little evidence of direct SARS-CoV-2 brain infection, although focal microvascular infection and ‘planted’ antigens have been suggested.
The study team performed detailed histopathology studies on the brains from 36 consecutive autopsies of patients who were RT-PCR positive for SARS-CoV-2.
Immunostaining for serum proteins, complement components and virus, as well as viral in-situ hybridization, were employed. The Mann-Whitney U test was used to compare activation of complement in brain microvessels in COVID-19 cases with immunostaining findings in pre-pandemic autopsy brains.
Alarmingly, neuropathologic findings in this COVID-19 cohort identified widespread reactive microvasculopathy (ectasia, mural distortion, and intussusceptive arborization) and acute intraluminal neutrophilic endotheliitis in the microcirculation in all 36 cases.
Prominent vascular neutrophilic transmural migration was found in several cases where it was best identified in larger microvessels.
In 25 cases there was acute microcirculatory perivasculitis. Activation of complement components, which included membrane attack complex, was significantly higher in microvascular walls in the COVID-19 cohort than in pre-pandemic cases.
The study findings suggest that in COVID-19 patients reactive microvasculopathy most likely originates from hypoxia, hypercytokinemia, and RAS dysfunction, while direct and indirect virus-induced factors may contribute.
Corresponding author, Dr Roy H. Rhodes from Louisiana State University Health Sciences Center told Thailand
Medical News, “Acute endothelitis, transmural migration, and acute perivasculitis constitute the early phase of type 3 hypersensitivity vasculitis in all of the cohort cases.”
Furthermore, the presence of activated complement components in microvascular walls in COVID-19 autopsy cases compared to controls is consistent with type 3 hypersensitivity vasculitis. Viral antigen in or ‘planted’ on microvessels or other antigen-antibody complexes could cause of this type of autoimmune vasculitis proximate to death. Coupling of neurogliovascular units could be compromised, if only temporarily in various brain regions, during the progression (initiation to healing) of these microvascular findings even in the absence of thrombosis or mural dehiscence. However, no specific neurological alteration in this cohor
t can be attributed directly to specific histopathologic findings.
The study findings were published on a preprint server and is currently being peer reviewed for publication in the journal: BMC Diagnostic Pathology.
https://www.researchsquare.com/article/rs-1619440/v1
Numerous past studies related to SARS-CoV-2 coronavirus have shown that the virus adversely affects major organs, e.g., the central nervous system (CNS).
The virus is the causal agent of the ongoing COVID-19) pandemic, which has already infected more than 518 million individuals globally and killed more than 6.25 million people to date according to reported figures. (In reality, the actual figures can be 4 to 5-fold!)
Studies have shown that SARS-CoV-2 infections causes CNS lesions associated with hemorrhage, encephalitis, encephalopathy, etc. Additionally, detection of SARS-CoV-2 proteins in the brain tissues via immunostaining suggested the presence of virions in the brain parenchyma as well as in the vascular endothelial cells.
Many researchers have suggested that the introduction of CNS lesions in COVID-19 patients might have occurred due to SARS-CoV-2 invasion via olfactory apparatus or infection of vascular endothelial cells. Further, the CNS could also be indirectly damaged in COVID-19 patients through coagulopathy, hypoxia due to pulmonary disease, or dysregulation in the renin-angiotensin system (RAS) owing to the viral infection.
Past studies have also shown that cytokine storm or hypercytokinemia could cause CNS damage. Although several studies have indicated the indirect effect of COVID-19 on CNS, scarce evidence is available regarding the direct effect of SARS-CoV-2 on brain infection.
This new study only focused on the microcirculatory factors associated with neurological complications of COVID-19.
The study team performed histopathology of the brains obtained from thirty-six consecutive autopsies of COVID-19 patients. All the study candidates showed positive RT-PCR for SARS-CoV-2. In the current study, immunostaining was conducted for serum proteins, complement components, and the virus.
The study team additionally performed viral in situ hybridization studies. The authors used the Mann-Whitney U test to compare activation of complement in brain microvessels in COVID-19 samples with immunostaining findings of pre-pandemic autopsy brains.
All thirty-six autopsy cases were of middle-aged to elderly adults. Both the genders were almost equally represented, and most of the candidates exhibited hypoxia. However, the clinical progression of the disease varied considerably in terms of length and complexity.
It was noted that the majority of patients were hypertensive, and over half of the cohort had suffered from diabetes mellitus, obesity, chronic heart condition, and a history of cancer or pulmonary disease. Interestingly, over half of the cohort consisted of African American ethnicity. However, owing to the small size of the study cohort, ethnicity was not an influencing factor.
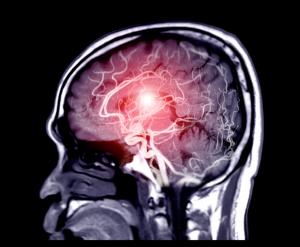
It should also be noted that in the brain’s microcirculatory system, normal CNS blood vessels’ (microvessels and capillaries) diameter ranges between 40 and 400 µm. Previous studies indicated that although CNS microcirculation could not be directly detected via magnetic resonance imaging (MRI), specific imaging methods are able to procure brain microvasculopathy in COVID-19 patients.
The study team reported the presence of both reactive and acute inflammatory microcirculatory alterations in all thirty-six COVID-19 autopsy cases. Past research indicated some conditions that lead to microcirculatory injury from COVID-19, which were hypoxia, RAS dysfunction, and hypercytokinemia. A prior study linked CNS microcirculation with endocytosed pseudovirions, which might have been formed by SARS-CoV-2 protein and associated with vascular endothelial cells.
The study findings indicated many microscopic sections to be unusual, and the majority of the samples were distorted, dilated, and had thin-walled microcirculatory channels. The study team stated that stalled microcirculatory healing in the brain during severe hypoxia might be enhanced by hypercytokinemia in COVID-19. Acute endotheliitis was found in half of the study cohort in two of the three major brain regions. Additionally, it was present in the brainstem of all but one patient.
The study team Researchers stated that acute endotheliitis is an autoimmune vasculitis, which is present in the initial phase of type 3 hypersensitivity vasculitis. The finding of a previous study is consistent with the current study that revealed karyorrhectic polymorphonuclear leukocytes (PMNs) in autoimmune vasculitis led to the recruitment of mononuclear cells in small-vessel vasculitis.
The study team reported that acute perivasculitis was present in 72.2% of the study cohort. They stated that more research is required to confirm the likelihood of circulating and planting SARS-CoV-2 proteins in the brain’s microcirculatory channels. Interestingly, 50% of the study cohort indicated induction of microcirculatory stress due to the presence of megakaryocytes in cerebral capillaries in COVID-19 cases.
The study findings confirmed the widespread prevalence of reactive and acute inflammatory CNS microvasculopathy in thirty-six COVID-19 brain autopsies. Owing to the scarce neurologic reports following hospitalization due to severe COVID-19 infection, the study team failed to provide the clinical correlation with histopathologic findings. However, previous findings indicated that hypoxia, hypercytokinemia, and RAS dysfunction have mostly caused reactive microvasculopathy in COVID-19 patients.
For more on
SARS-CoV-2 Effects On The Brains, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/new-non-human-primate-study-alarmingly-reveals-that-sars-cov-2-infections-can-lead-to-brain-inflammation,-brain-hypoxia,-brain-bleeding-and-also-strok