BREAKING! Study Shows That Immune Cells Called Macrophages Show Altered Inflammatory And Metabolic Expression Several Months After Mild COVID-19!
Source: Medical News - Immune Inflammation Mar 15, 2022 3 years, 9 months, 4 weeks, 1 day, 6 hours, 19 minutes ago
A new study by researchers from the Helmholtz Center Munich (HMGU)-Germany, Technical University of Munich (TUM)-Germany and Karolinska Institutet-Sweden has alarming found that immune cells called macrophages show altered inflammatory and metabolic expression several months after mild SARS-CoV-2 infections! The study team was surprised to see persistent elevation of inflammation in the immune cells of individuals that only had mild COVID-19 symptoms upon infection, in many cases lasting for very long periods of time.
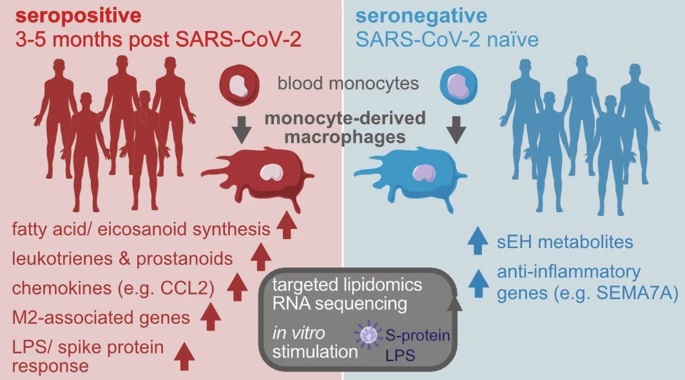
Monocyte-derived macrophages (MDM) drive the inflammatory response to SARS-CoV-2infections and are a major source of eicosanoids in airway inflammation.
The study team reported that monocyte-derived macrophages or MDM from SARS-CoV-2-infected individuals with mild disease show an inflammatory transcriptional and metabolic imprint that lasts for at least 5 months after SARS-CoV-2 infection!
Interestingly, monocyte-derived macrophages or MDM from convalescent SARS-CoV-2-infected individuals showed a downregulation of pro-resolving factors and an increased production of pro-inflammatory eicosanoids, particularly 5-lipoxygenase-derived leukotrienes.
It was found that leukotriene synthesis was further enhanced by glucocorticoids and remained elevated at 3–5 months, but had returned to baseline at 12 months post SARS-CoV-2 infection. Stimulation with SARS-CoV-2 spike protein or LPS triggered exaggerated prostanoid-, type I IFN-, and chemokine responses in post COVID-19 MDM.
The study findings show that SARS-CoV-2 infection leaves an inflammatory imprint in the monocyte/ macrophage compartment that drives aberrant macrophage effector functions and eicosanoid metabolism, resulting in long-term immune aberrations in patients recovering from mild COVID-19.
The study findings were published in the peer reviewed journal: Mucosal Immunology.
https://www.nature.com/articles/s41385-021-00482-8
To date, there is still a lack of understanding as to why some individuals suffer from long-lasting symptoms after a SARS-CoV-2 infection.
This is the first study to demonstrate that a certain type of immune cells called macrophages show altered inflammatory and metabolic expression several months after mild COVID-19.
Co-Author Dr Craig Wheelock, a docent at the Department of Medical Biochemistry and Biophysics at Karolinska Institutet told Thailand
Medical News, "Our study findings show that the macrophages from individuals with mild COVID-19 exhibit an altered inflammatory and metabolic expression for three to five months post-infection. Although most of these individuals do not have any persistent symptoms, their immune system are more sensitive than that of their healthy counterparts.”
He further added, that individuals having such an immune state could be more vulnerable to reinfections and also to other secondary opportunistic infections and also are more prone to a variety of health conditions.
Although long-term symptoms are relatively common after a severe COVID-19 infection, it may also affect individuals with previous mild disease.
In
fact, of late, long term symptoms are seen rising in not only those who had initial mild symptoms but also in those who were asymptomatic!
Further detailed research is needed to understand the long-term immune aberrations in patients who have recovered from the acute phase of the infection.
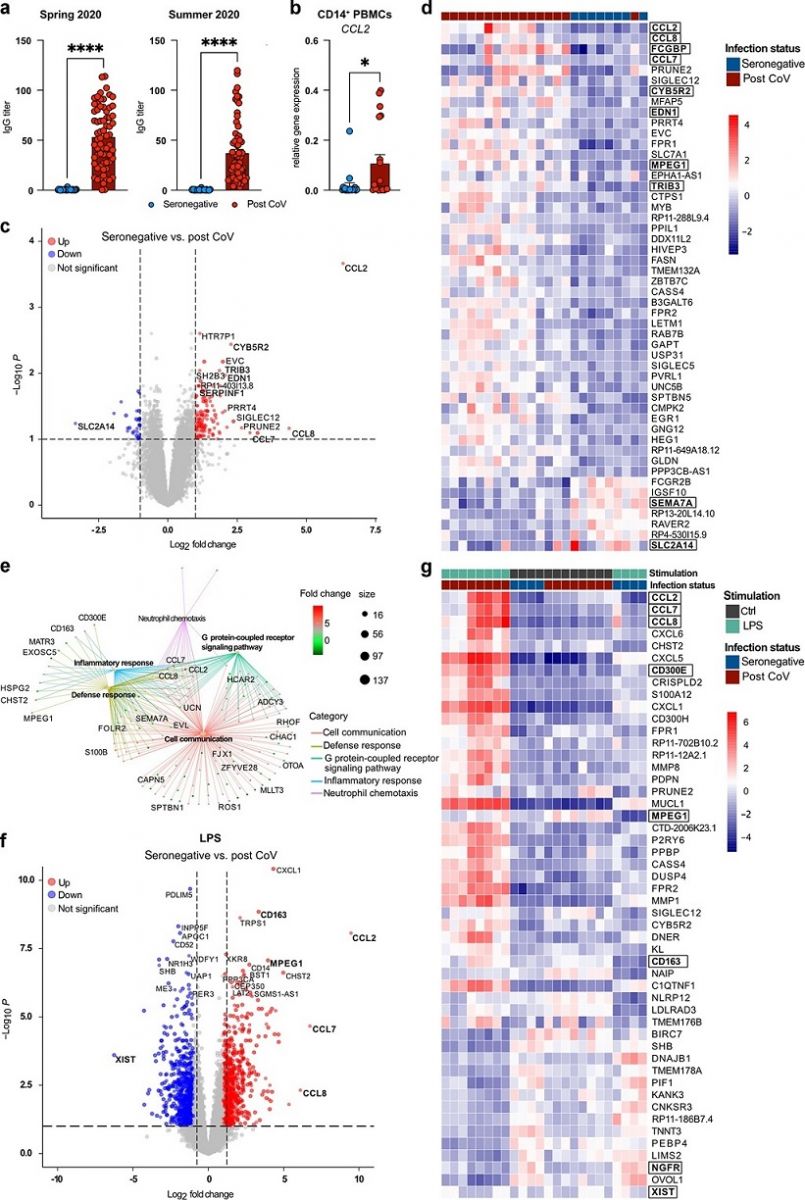 a Serum IgG titers of seronegative (n = 36) or SARS-CoV-2 seropositive (post CoV) (n = 68) individuals in Spring 2020 or at 3–5 months post infection (p.i.) (Summer 2020). Data are shown as mean + SEM. b Expression of CCL2 in CD14+ PBMCs of seronegative (n = 20) vs. post CoV (n = 19) subjects at 3–5 months p.i. c Volcano plot showing DEGs between seronegative (n = 8) and post CoV MDM (n = 16). Top 10 DEGs (base mean > 50), log2 FC > 2 or adjusted p value (padj < 0.016 labeled), DEGs with log2 FC > 1 and padj < 0.1 marked. d Heatmap of top 50 DEGs between seronegative (n = 8) and post CoV (n = 16) MDM, padj < 0.1, log2 FC > 1; base mean > 50. e GSEA between post CoV (n = 8) and seronegative (n = 4) MDM + LPS, log2 FC > 2, p value < 0.01. f Volcano plot showing DEGs between seronegative (n = 4) and post CoV (n = 8) MDM + LPS. DEGs with log2 FC > 3 or padj < 1 × 10−6 labeled, DEGs with log2 FC > 1 and padj < 0.1 marked. g Heatmap of top 50 DEGs between seronegative (n = 4) and post CoV (n = 8) MDM ± LPS, padj < 0.1, log2 FC > 1, base mean > 50. Statistical significance was determined by Mann–Whitney test (a, b) or DESeq2 (c–f). *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001.
a Serum IgG titers of seronegative (n = 36) or SARS-CoV-2 seropositive (post CoV) (n = 68) individuals in Spring 2020 or at 3–5 months post infection (p.i.) (Summer 2020). Data are shown as mean + SEM. b Expression of CCL2 in CD14+ PBMCs of seronegative (n = 20) vs. post CoV (n = 19) subjects at 3–5 months p.i. c Volcano plot showing DEGs between seronegative (n = 8) and post CoV MDM (n = 16). Top 10 DEGs (base mean > 50), log2 FC > 2 or adjusted p value (padj < 0.016 labeled), DEGs with log2 FC > 1 and padj < 0.1 marked. d Heatmap of top 50 DEGs between seronegative (n = 8) and post CoV (n = 16) MDM, padj < 0.1, log2 FC > 1; base mean > 50. e GSEA between post CoV (n = 8) and seronegative (n = 4) MDM + LPS, log2 FC > 2, p value < 0.01. f Volcano plot showing DEGs between seronegative (n = 4) and post CoV (n = 8) MDM + LPS. DEGs with log2 FC > 3 or padj < 1 × 10−6 labeled, DEGs with log2 FC > 1 and padj < 0.1 marked. g Heatmap of top 50 DEGs between seronegative (n = 4) and post CoV (n = 8) MDM ± LPS, padj < 0.1, log2 FC > 1, base mean > 50. Statistical significance was determined by Mann–Whitney test (a, b) or DESeq2 (c–f). *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001.
In order to examine this aspect, the study team in the current research analyzed blood samples from 68 people with previous mild COVID-19 infection and a control group of 36 people who had not had COVID-19.
The study team isolated the macrophages in the laboratory and stimulated them with spike protein, steroids and lipopolysaccharides (LPS), a molecule that triggers the immune system. The cells were then RNA-sequenced to measure active genes.
The study team also measured the presence of eicosanoid signaling molecules, which are a fundamental feature of inflammation.
Dr Wheelock added, "Typically it is not surprising to find a large number of eicosanoid molecules in individual with COVID-19 as the disease causes inflammation, but it was shocking that they were still being produced in high quantities several months after the infection.”
The research findings also showed a higher concentration of leukotrienes, which are a type of pro-inflammatory molecules known for causing asthma.
Corresponding author Dr Julia Esser-von Bieren from the Helmholtz Center Munich and the Technical University of Munich further added, "It's very striking that the concentration of leukotrienes remains elevated in macrophages in individuals who have had mild COVID-19. Leukotrienes are key mediators of asthma, but they're also involved in the antiviral host defense against influenza. A sustained increase after SARS-CoV-2 infection could cause a greater sensitivity to respiratory inflammation, but could also improve antiviral immunity to SARS-CoV-2 or other viruses."
For the study, all the blood specimens were collected on two occasions, at three to five months after SARS-CoV-2 infection and after 12 months.
It was reported that at three to five months, around 16 percent reported persistent mild symptoms while the rest were symptom-free.
However, at 12 months, none reported persistent symptoms and there was no longer any difference in inflammatory markers between those with previous COVID-19 infection and the healthy control group.
The study team notes that the post-COVID diagnosis was not specifically examined in the study and as such more research is needed to determine if these results can be directly linked to what is also known as long COVID.
Dr Esser-von Bieren added, "We would like to do a corresponding study in which we involve both individuals with severe COVID-19 and individuals without COVID-19 but who have another kind of respiratory disease, such as influenza. We'll then examine if what inflicts COVID-19 patients also inflicts those with, say, seasonal influenza."
The study team warned, “The persistent upregulation of pro-inflammatory eicosanoids in post COVID-19 macrophages may have multiple consequences for subsequent immune responses, e.g. during bacterial or viral infection or in patients suffering from chronic inflammatory diseases such as asthma, thus requiring future investigation.”
For more on
Immune Inflammation in Post Mild-COVID-19, keep on logging to Thailand Medical News.
 a Serum IgG titers of seronegative (n = 36) or SARS-CoV-2 seropositive (post CoV) (n = 68) individuals in Spring 2020 or at 3–5 months post infection (p.i.) (Summer 2020). Data are shown as mean + SEM. b Expression of CCL2 in CD14+ PBMCs of seronegative (n = 20) vs. post CoV (n = 19) subjects at 3–5 months p.i. c Volcano plot showing DEGs between seronegative (n = 8) and post CoV MDM (n = 16). Top 10 DEGs (base mean > 50), log2 FC > 2 or adjusted p value (padj < 0.016 labeled), DEGs with log2 FC > 1 and padj < 0.1 marked. d Heatmap of top 50 DEGs between seronegative (n = 8) and post CoV (n = 16) MDM, padj < 0.1, log2 FC > 1; base mean > 50. e GSEA between post CoV (n = 8) and seronegative (n = 4) MDM + LPS, log2 FC > 2, p value < 0.01. f Volcano plot showing DEGs between seronegative (n = 4) and post CoV (n = 8) MDM + LPS. DEGs with log2 FC > 3 or padj < 1 × 10−6 labeled, DEGs with log2 FC > 1 and padj < 0.1 marked. g Heatmap of top 50 DEGs between seronegative (n = 4) and post CoV (n = 8) MDM ± LPS, padj < 0.1, log2 FC > 1, base mean > 50. Statistical significance was determined by Mann–Whitney test (a, b) or DESeq2 (c–f). *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001.
a Serum IgG titers of seronegative (n = 36) or SARS-CoV-2 seropositive (post CoV) (n = 68) individuals in Spring 2020 or at 3–5 months post infection (p.i.) (Summer 2020). Data are shown as mean + SEM. b Expression of CCL2 in CD14+ PBMCs of seronegative (n = 20) vs. post CoV (n = 19) subjects at 3–5 months p.i. c Volcano plot showing DEGs between seronegative (n = 8) and post CoV MDM (n = 16). Top 10 DEGs (base mean > 50), log2 FC > 2 or adjusted p value (padj < 0.016 labeled), DEGs with log2 FC > 1 and padj < 0.1 marked. d Heatmap of top 50 DEGs between seronegative (n = 8) and post CoV (n = 16) MDM, padj < 0.1, log2 FC > 1; base mean > 50. e GSEA between post CoV (n = 8) and seronegative (n = 4) MDM + LPS, log2 FC > 2, p value < 0.01. f Volcano plot showing DEGs between seronegative (n = 4) and post CoV (n = 8) MDM + LPS. DEGs with log2 FC > 3 or padj < 1 × 10−6 labeled, DEGs with log2 FC > 1 and padj < 0.1 marked. g Heatmap of top 50 DEGs between seronegative (n = 4) and post CoV (n = 8) MDM ± LPS, padj < 0.1, log2 FC > 1, base mean > 50. Statistical significance was determined by Mann–Whitney test (a, b) or DESeq2 (c–f). *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001.