BREAKING! U.S. Medical News: First Case Of Opportunistic Pneumonia In An American COVID-19 Patient Involving The Rare Fungus Trichosporon Asahii!
U.S. Medical News - COVID-19 - Opportunistic Pneumonia - Trichosporon Asahii Jan 26, 2023 2 years, 4 weeks, 2 days, 22 hours, 6 minutes ago
U.S. Medical News: Medical researchers from Loma Linda University Murrieta Campus, Murrieta, California-USA have reported the first documented case report of a COVID-19 patient with opportunistic pneumonia caused by the rare fungus: Trichosporon Asahii.
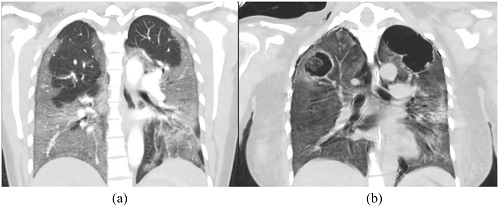
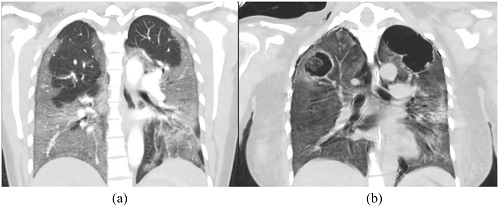 A) CT Chest with contrast on admission. B) CT chest without contrast on hospital day 20.
A) CT Chest with contrast on admission. B) CT chest without contrast on hospital day 20.
Trichosporon asahii (formerly Trichosporon beigelii) is an emerging fungal pathogen seen particularly in immunologically compromised patients and is a life-threatening yeast with no effective antifungal therapy available to date.
Trichosporon species differ from Candida species in several respects: they do not produce a germ tube, as does Candida albicans; they can form both hyaline septate hyphae as well as pseudohyphae; and they produce arthroconidia. Infections due to Trichosporon species may be superficial, involving hair shafts known as “white piedra,” or disseminated, involving ≥1 visceral organs, as a result of fungemia.
The organisms are found naturally in the soil and may also be part of the normal human flora in stool or skin. Risk factors for hematogenous spread that causes deep infections are use of immunosuppressive drugs and immunocompromised states.
Typically, it is found in patients with cancer. In fact, 80% of the ~100 reported cases of hematogenous T. asahii (formerly Trichosporon beigelii) infections have occurred in patients with leukemia, most of whom had neutropenia. Other, less common predisposing factors include HIV infection, burns, organ transplantation, and peritoneal dialysis.
It can disseminate into multiple organs and is associated with high mortality.
Common clinical features of disseminated infections include septic shock, pneumonia, renal failure, chorioretinitis, and cutaneous lesions. Skin lesions usually appear as scattered red papules, which may ulcerate and reveal fungal elements and vessel thrombosis on biopsy. Renal involvement may manifest as proteinuria and hematuria as well as renal failure.
https://academic.oup.com/cid/article/33/5/e28/470071
According to the study team, this is the first reported case of fatal opportunistic Trichosporon asahii pneumonia in the setting of severe COVID-19 pneumonia in the United States.
The patient had ventilator-requiring respiratory failure secondary to COVID-19-19 infection. The patient received intravenous broad-spectrum antibiotics, tocilizumab, and corticosteroids with subsequent development of cavitary infiltrates. Bronchoalveolar lavage grew T. asahii.
The study team described a rare complication of COVID-19 infection and describe the microbial diagnosis, possible mechanism of infection, and optimal treatment.
The case report was published in the peer reviewed journal: ID Cases by Science Direct.
https://www.sciencedirect.com/science/article/pii/S2214250923000252
While other
;U.S. Medical News outlets have not reported about Trichosporon Asahii in COVID-19 patients, Thailand Medical News would however like to note that opportunistic infections in COVID-19 patients especially those who are in severe conditions, involving the Trichosporon Asahii have also been reported in the past in the United States and also elsewhere, though not linked with pneumonia but rather infections of the urinary tract, bloodstream infection, etc
https://www.hindawi.com/journals/criid/2021/6841393/
https://www.sciencedirect.com/science/article/pii/S1130140622000201
https://link.springer.com/article/10.1007/s11046-022-00637-6
https://www.sciencedirect.com/science/article/pii/S2214250921002006
A Qatar study had also shown that Trichosporon Asahii was emerging as an invasive pathogen in critically ill COVID-19 patients.
https://www.sciencedirect.com/science/article/pii/S2214250921002006
In the current case study, a 36-year-old COVID-19 unvaccinated woman presented in April 2021, to a Southern California hospital for a five-day history of shortness of breath, cough, fever, and chills. She was diagnosed with COVID-19 infection and was admitted for acute hypoxic respiratory failure requiring supplemental oxygen. Her past medical history was significant for a BMI of 28 and diet-controlled diabetes (hemoglobin A1c 6.3%). She lived with her husband and two children and had no recent travel history. She reported vaping tobacco for 2 years and denied alcohol or recreational drug use. On admission, a chest CT angiogram showed bibasilar consolidations.
On day 3 at the hospital, her oxygen requirement escalated to 60 liters by high-flow nasal cannula. She received a 5-day course of intravenous (IV) remdesivir, a 10-day course of dexamethasone and one dose of tocilizumab 400 mg.
Her condition deteriorated and on hospital day eight she was transferred to the intensive care unit (ICU) and required intubation and mechanical ventilation. She developed multi-organ dysfunction syndrome with severe acute respiratory distress syndrome, septic shock, ischemic hepatitis, acute renal failure requiring hemodialysis, and left upper lobe pulmonary embolism. The patient received an empiric course of IV cefepime, metronidazole, vancomycin, and micafungin. Multiple blood cultures, bacterial and fungal sputum cultures, and urine cultures were negative. Serum aspergillus antigen and an interferon gamma assay were negative; beta-d-glucan was not available to order in the institution.
Even with broad antimicrobial therapy, the patient had a persistent leukemoid reaction and high oxygenation requirements. Repeat CT scan of the chest without contrast demonstrated bilateral upper lobe cavities which were not present on her prior CT scan. Bacterial culture of endotracheal aspirate on day 20 was negative. Fungal culture grew yeast with hyphae and arthroconidia identified by MALDI- TOF as T. asahii.
It was reported that on day 22, bronchoalveolar lavage (BAL) was performed yielding negative bacterial and mycobacterial cultures. BAL pneumocystis stain was negative. BAL fungal culture grew T. asahii. The patient was initially treated with IV liposomal amphotericin followed by voriconazole based on identification and susceptibility results. MICs were as follows: amphotericin (AMB) B 0.5 ug/mL, caspofungin > 8 ug/ml, fluconazole = 1ug/mL, posaconazole =0.125ug/mL, voriconazole = 0.06 ug/mL, and itraconazole = 0.5ug/mL. Despite aggressive medical therapy, the patient continued to deteriorate and expired on hospital day 37.
According to the study team, this is the first report of fatal pneumonia due to T. asahii as the sole microbial pathogen in the setting of severe COVID-19 infection. T. asahii has been linked to fungemia in critically ill COVID-19 patients, but pneumonia is rare. The delayed identification of T. asahii and the common use of echinocandins may contribute to increased morbidity and mortality. More clinical data are needed to optimize the diagnosis and treatment of severe Trichosporon infections.
While some may attribute certain drugs being used during treatment protocols as being behind the immunocompromised states arising and making patients susceptible to such opportunistic pathogens, Thailand Medical News would like to stress that it is the SARS-CoV-2 induced immune dysfunction and COVID-19 induced immunodeficiency that is responsible for such opportunistic infections and we can expect o see a rise of more cases of Trichosporon Asahii opportunistic infections in both severe and also post COVID patients soon.
For the latest
U.S. Medical News, keep on logging to Thailand Medical News.