BREAKING! University Of Oxford Study Shockingly Finds That Lungs of Post COVID-19 Individuals Displayed Premature Aging Of More Than 15 Years!
Source: Long COVID - Premature Aging Of Lungs Oct 04, 2022 3 years, 3 months, 2 days, 15 hours, 3 minutes ago
Long COVID: A study by researchers from University of Oxford- United Kingdom involving a new computational technique has shockingly revealed that the lungs of Post COVID-19 individuals displayed premature aging of more than 15 years along with other lung dysfunctions!
To date, the long-term effects of COVID-19 on lung physiology remain poorly understood.
The study team utilized a new computational technique involving computed cardiopulmonography (CCP) to study two COVID-19 cohorts (MCOVID and C-MORE-LP) at both ~6 and ~12 months post infection.
MCOVID is a a cohort of military personnel and C-MORE-LP is a cohort derived from the general patient population (Capturing MultiORgan Effects of COVID-19 Lung Physiology)
CCP is comprised of two components. The first is to collect highly precise, highly time-resolved measurements of gas exchange using a purpose-built molecular flow sensor based around laser absorption spectroscopy. The second component is to estimate physiological parameters by fitting a cardiopulmonary model to the dataset. The measurement protocol involved 7 min breathing air followed by 5 min breathing pure O2.
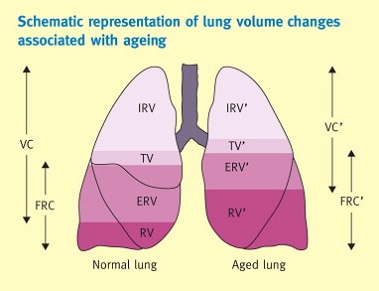
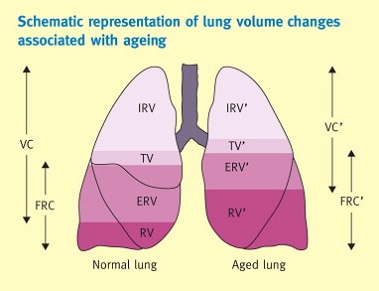
A total of 178 participants were studied, with 97 returning for a repeat assessment. 126 arterial blood gas samples were drawn from MCOVID participants. For participants who had required intensive care and/or invasive mechanical ventilation, there was a significant increase in anatomical deadspace of ~ 30 ml and a significant increase in alveolar-to-arterial PO2 gradient of ~ 0.9 kPa relative to controls. Those who had been hospitalized had reductions in functional residual capacity of ~ 15%.
Shockingly, the study findings showed that irrespective of COVID-19 severity, participants who COVID-19 demonstrated a modest increase in ventilation inhomogeneity, broadly equivalent to that associated with 15 years of aging!
The research also illustrates the capability of CCP to study aspects of lung function not so easily addressed through standard clinical lung function tests.
The study findings were published in the peer reviewed Journal of Applied Physiology.
https://journals.physiology.org/doi/abs/10.1152/japplphysiol.00436.2022
It is already known that as a respiratory disease, SARS-CoV-2 infection mainly affects the lungs.
Although most individuals recover completely, a significant number of individuals experience symptoms that can persist for weeks or months post COVID infection, sometimes referred to as "long COVID."
To date, it remains unclear whether these symptoms are associated with any long-term damage that reduces the function of the lungs and respiratory system.
In order to investigate this, the study team utilized a new computational approach to assess how COVID-19 may affect long-term lung function.
The
Long COVID research was based on 178 participants who were grouped into four categories:
1. Control participants, who ha
d not had COVID-19;
2. Those who had COVID-19 and were managed in the community;
3. Those who were hospitalized with COVID-19 but not admitted to an intensive care unit (ICU);
4. Those who were admitted to an ICU with severe COVID-19 and in most cases received invasive mechanical ventilation.
The research participants were studied six months and twelve months after SARS-CoV-2 infection, utilizing a novel computational approach to assess lung function.
The study findings showed that prior COVID-19 infection was associated with more uneven inflation of the lungs during normal breathing. This is something that is part of normal aging in the lung. The changes seen after COVID-19 in this study are roughly equivalent to those associated with 15 years of normal aging, but are still much smaller than those seen in established lung disease!
The findings also revealed that there was an association between hospitalization with COVID-19 and smaller lung volumes, but it is not known whether the smaller volumes are caused by COVID-19 infection, or instead represent a predisposing factor for more severe infection.
It was also found that admission to the ICU was associated with an enlarged respiratory dead space (the volume of gas that is breathed into the lungs but does not participate in gas exchange). This may have been caused by COVID-19 infection, but equally may have been caused by the process of mechanical ventilation.
The study team assessed lung function utilized a novel technique called computed cardiopulmonography.
In the novel approach, study participants breathe through a mouthpiece connected to the measuring device that uses lasers to take highly precise measurements of gas composition. These measurements are then fed into a computational model of the respiratory and cardiovascular systems to estimate values for aspects relating to the individual's lung function. For each individual, the model was adjusted to take into account physiological factors that can influence lung function, such as sex, age, height, and body mass.
This novel technique has already been shown capable of predicting whether patients with asthma required an increase in their medication. It also shows promise as a method to detect sub-clinical lung disease, opening the possibility of eventually treating patients earlier to prevent the onset of more significant disease.
Dr Peter Robbins, a professor from the University of Oxford's Department of Physiology, Anatomy and Genetics who is also the lead author told Thailand Medical News, "Our research illustrates the capability of this novel technique to study aspects of lung function not so easily measured through standard clinical tests. However, without measurements prior to infection, it is not possible to conclude whether these differences result directly from COVID-19 infection, or whether they are actual risk factors associated with the lungs that predispose towards more serious disease."
Dr Nayia Petousi, a respiratory consultant from the University of Oxford's Nuffield Department of Medicine and one of the clinical leads for the study added, "We hope that by providing insight into the understanding of post-COVID effects on the lungs the results can be of help in the clinical management of patients."
For the latest
Long COVID Research, keep on logging to Thailand
Medical News.