BREAKING! University of Wisconsin-Madison Study Shockingly Reveals Antibody-Dependent Enhancement of SARS-CoV-2 Infection Mediated By IgG Receptors!
Source: SARS-CoV-2 ADE Sep 30, 2021 3 years, 6 months, 4 days, 4 hours, 53 minutes ago
ADE and SARS-CoV-2 Variants: A new study by researchers from University of Wisconsin-Madison has shockingly revealed that Antibody-Dependent Enhancement of SARS-CoV-2 Infection Is mediated by the IgG Receptors FcγRIIA and FcγRIIIA but does not contribute to aberrant cytokine production by macrophages.
The study also warns that the new emerging SARS-CoV-2 variants could actually contribute more in terms of the
ADE phenomena in terms of those that had already been infected with the earlier strains of the SARS-CoV-2 or had even been vaccinated! (My predictions are coming true and my prayers are beginning to be answered!)
Numerous questions have been raised about the detrimental effects of antibodies during this COVID-19 pandemic considering that it was widely seen in 2003 SARS-CoV.
Antibody-dependent enhancement (ADE) of infection is one of the biggest concerns in terms of not only the antibody reaction to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) upon reinfection with the virus but also the reaction to COVID-19 vaccines.
The study team evaluated ADE of infection by using COVID-19 convalescent-phase plasma and BHK cells expressing human Fcγ receptors (FcγRs).
The study team shockingly found that FcγRIIA and FcγRIIIA mediated modest ADE of infection against SARS-CoV-2. Although ADE of infection was observed in monocyte-derived macrophages infected with SARS-CoV-2, including its variants, proinflammatory cytokine/chemokine expression was not upregulated in macrophages. SARS-CoV-2 infection thus produces antibodies that elicit ADE of infection, but these antibodies do not contribute to excess cytokine production by macrophages.
It is important to note that viruses infect cells mainly via specific receptors at the cell surface. Antibody-dependent enhancement (ADE) of infection is an alternative mechanism of infection for viruses to infect immune cells that are mediated by antibodies and IgG receptors (FcγRs).
Because ADE of infection contributes to the pathogenesis of some viruses, such as dengue virus and feline coronavirus, it is important to evaluate the precise mechanism of ADE and its contribution to the pathogenesis of SARS-CoV-2.
In this study using convalescent-phase plasma from COVID-19 patients, the study team found that two types of FcγRs, FcγRIIA and FcγRIIIA, mediate ADE of SARS-CoV-2 infection. Although ADE of infection was observed for SARS-CoV-2 and its recent variants, proinflammatory cytokine production in monocyte-derived macrophages was not upregulated.
The study findings suggest that SARS-CoV-2 infection produces antibodies that elicit ADE of infection, but these antibodies may not be involved in aberrant cytokine release by macrophages during SARS-CoV-2 infection.
The study findings were published in the journal: mBio (Published by the American Society For Microbiology.)
https://journals.asm
.org/doi/10.1128/mBio.01987-21
The COVID-19 pandemic wreaked havoc around the world, leading to lockdowns, social distancing measures, and millions of deaths. However, with the help of mass vaccination campaigns and monoclonal antibody treatments, the transmission of the disease is beginning to slow down.
All vaccines rely on the immune system’s ability to produce specific antibodies ie most vaccines are designed to inhibit the SARS-CoV-2 by targeting the receptor-binding domain (RBD) of the S1 subunit of the spike protein, as this is responsible for viral cell entry through binding to the angiotensin-converting enzyme 2 (ACE2).
It should be noted that however that some viruses especially coronaviruses (including SARS-CoV-2) have an alternative method of infection known as an antibody-dependent enhancement of infection (ADE).
It is one of the most significant risks and threats for both vaccines and monoclonal antibody treatment and is of special concern given the rise of variants of concern such as the Delta variant which is known to evade vaccine-induced immunity.
Typically in ADE, an immune complex of virus and non-neutralizing or cross-reactive antibodies binds to receptor molecules called Fcy receptors (FcyRs) on macrophages and monocytes. These cells then internalize the complex, allowing the virus to enter the cell.
Importantly both SARS-CoV-1 and MERS-CoV showed the ability to enter cells through ADE, and several studies have confirmed that SARS-CoV-2 has the same ability using FcyRIIA. Still, it is unknown whether FcyRIA or FcyRIIIA are also involved until this new study finding.
https://pubmed.ncbi.nlm.nih.gov/32908214/
https://pubmed.ncbi.nlm.nih.gov/32659783/
The study team generated baby hamster kidney (BHK) cells expressing the three FcyRs or ACE2. Wild-type BHK cells are not susceptible to infection by SARS-CoV-2, and as such, they make an ideal model to test whether the transfected proteins mediate ADE.
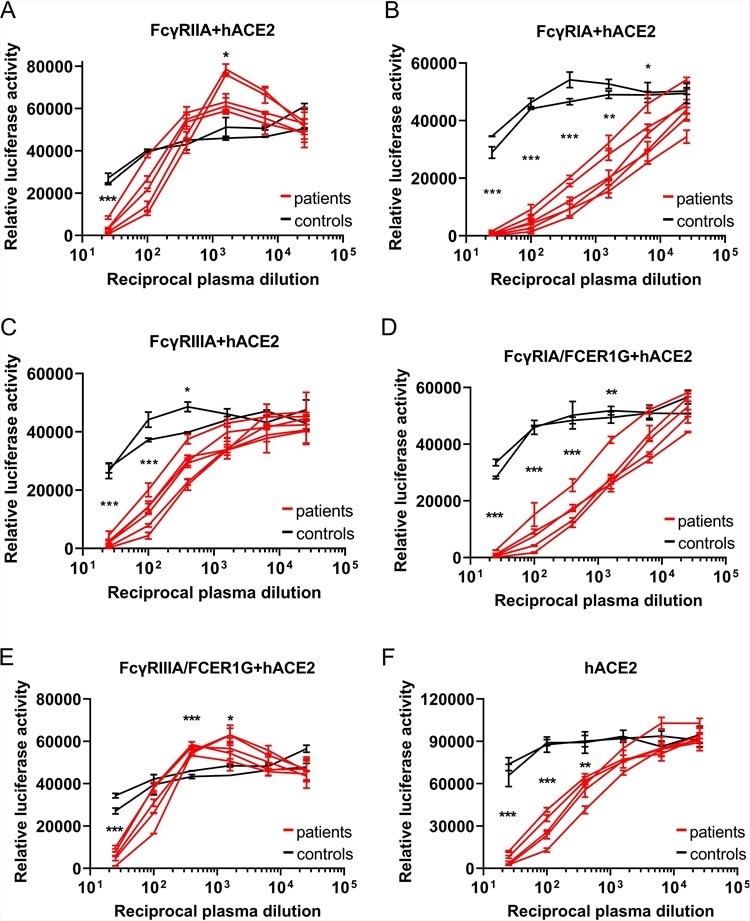
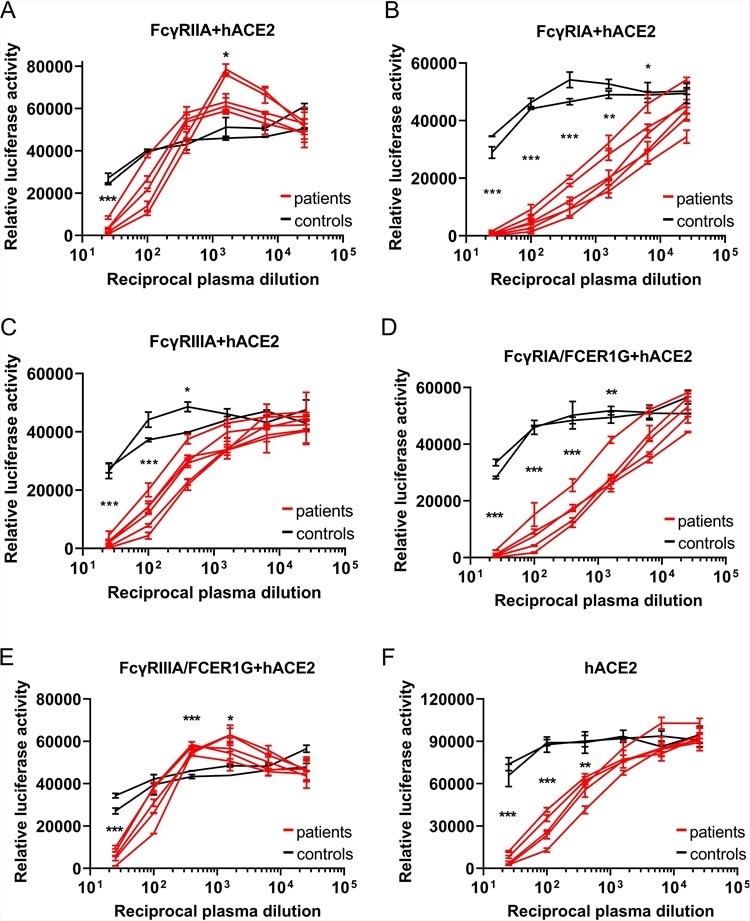 Graphs showing that ADE of SARS-CoV-2 infection is mainly mediated by FcγRIIA and FcγRIIIA. (A to E) Serially diluted convalescent-phase plasma from five individuals and two control plasma samples incubated with VSV-SARS2-S were used to infect the indicated cells that had been transfected with an hACE2 expression vector; the luciferase activity in the cell lysates was determined at 24 hpi. The experiment was performed with duplicate samples; means and standard deviations (SD) are shown. (F) Serially diluted convalescent-phase plasma from two individuals and two control plasma samples incubated with VSV-SARS2-S were used to infect the indicated cells, and the luciferase activity in the cell lysates was determined at 24 hpi. The experiments were performed in duplicate; means and SD are shown. Statistical analysis was performed using an unpaired t test. ***, P < 0.001; **, P < 0.01; *, P < 0.05.
Graphs showing that ADE of SARS-CoV-2 infection is mainly mediated by FcγRIIA and FcγRIIIA. (A to E) Serially diluted convalescent-phase plasma from five individuals and two control plasma samples incubated with VSV-SARS2-S were used to infect the indicated cells that had been transfected with an hACE2 expression vector; the luciferase activity in the cell lysates was determined at 24 hpi. The experiment was performed with duplicate samples; means and standard deviations (SD) are shown. (F) Serially diluted convalescent-phase plasma from two individuals and two control plasma samples incubated with VSV-SARS2-S were used to infect the indicated cells, and the luciferase activity in the cell lysates was determined at 24 hpi. The experiments were performed in duplicate; means and SD are shown. Statistical analysis was performed using an unpaired t test. ***, P < 0.001; **, P < 0.01; *, P < 0.05.
The BHK cells were infected with a luciferase-expressing vesicular stomatitis virus pseudotyped with SARS-CoV-2 spike (VSV-SARS2-S). Luciferase activity was evaluated 24 hours post-transfection.
Only the BHK cells that were expressing ACE2 proved susceptible to VSV-SARSS2-S transfection.
Following this, the study team used 15 convalescent-phase plasma samples randomly selected from a total of 110 samples, and one sample from an uninfected individual. The transfected FcyR BHK cells were then infected with VSV-SARSS2-S that had been incubated with these samples.
No luciferase signals were detected at all, suggesting none of the FcyRs mediate ADE in BHK cells.
Shockingly however, in FcyR BHK cells transfected with ACE2, luciferase levels were significantly higher when infected with VSV-SARS2-S incubated with increasingly diluted plasma, indicating that the FcyR enhanced VSV-SARS2-S infection.
This was fortunately only seen with FcyRIIA, and not the other two receptors.
In order to further investigate the possibility of ADE in SARS-CoV-2 infection, the study team explored the possibility that an association with the FcRy subunit was required for the function of FcyRIA and FcyRIIIA.
The team engineered the BHK cells expressing those receptors once again, this time in order to allow them to express FCERIG (the subunit involved) stably.
Interestingly there was a significant increase in luciferase signals for FcyRIIIA-FCER1G BHK cells, suggesting that the FCERIG was necessary for activation.
As no ADE of infection was detected in hACE2-BHK cells, these data suggest that ADE can aid SARS-CoV-2 infection in humans.
Importantly upon expanding the testing to include convalescent-phase plasma obtained 1, 3, and 6 months post-diagnosis all showed positive results. These tests were repeated with primary human macrophages, but no SARS-CoV-2 replication was found.
The study team proposes that their results prove that SARS-CoV-2 infection induces antibodies that can cause ADE-induced infection, and that these antibodies persist for six months post-infection at a minimum.
The study team highlights the importance of their study given the emergence of multiple variants of concern, especially as the risk of reinfection could trigger a worse prognosis. This is because the variants antigenicity is different from the original strain found in Wuhan, China.
Hence the findings show that while an infected individual will still have a robust immune reaction, it will be less effective against the new strain while also paving the way for ADE-induced infection.
The study findings are backed up by several studies, including similar results for SARS-CoV-2 replication in macrophages
https://www.thailandmedical.news/news/breaking-yale,-harvard-rockefeller-study-discovers-that-sars-cov-2-is-able-to-enter-replicate-in-human-host-macrophages,triggering-inflammatory-cascad
and a finding of a correlation between ADE-inducing antibodies and COVID-19 severity.
Significantly, the emerging worrisome variants of concern appear even more dangerous with this new information.
As of press time, the WHO, the US CDC and four different vaccine manufacturers refused to comment when asked about these new study findings.
For more about
ADE and SARS-CoV-2 Variants, keep on logging to Thailand Medical News.