Breakthrough! University Of Alabama Study Finds That The Drug To Treat Blood Cancer-Venetoclax Could Be Repurposed To Reverse Lung Fibrosis Especially In COVID!
Source: Pulmonary Fibrosis Sep 01, 2021 4 years, 3 months, 3 weeks, 5 days, 22 hours, 40 minutes ago
A new breakthrough study by researchers from University of Alabama at Birmingham-USA has found that the drug Venetoclax used to treat adult patients with Chronic Lymphocytic Leukemia (CLL) could be repurposed to reverse lung fibrosis after successful mouse model drug trials.
Venetoclax, sold under the brand names Venclexta and Venclyxto, is a medication used to treat adults with chronic lymphocytic leukemia, small lymphocytic lymphoma, or acute myeloid leukemia. The most common side effects are low levels of neutrophils, diarrhea, nausea, anemia, nose and throat infection and tiredness. Although initially expensive, the generic versions of the drug are now available cheaply in Vietnam and India.
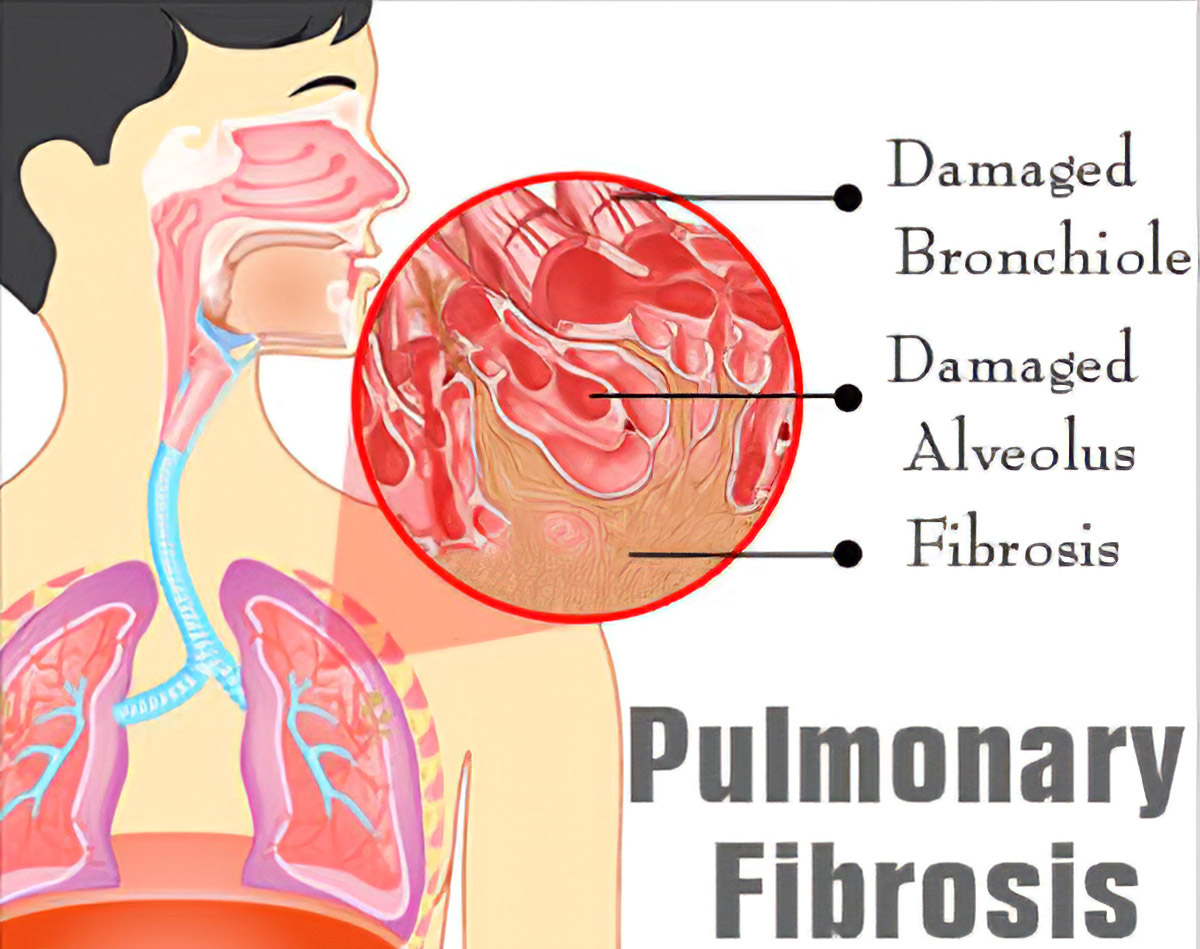
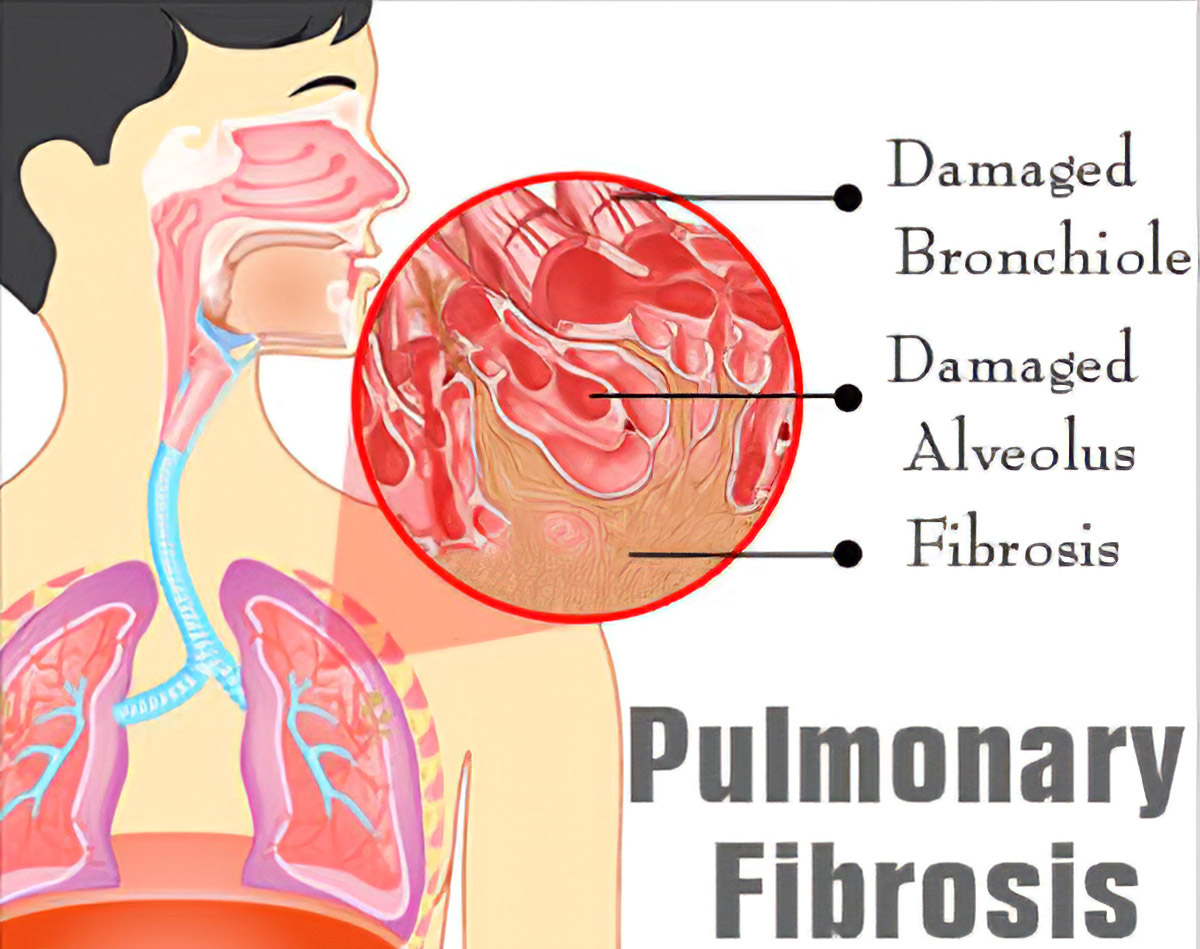
Pulmonary fibrosis is a condition in which the lungs become scarred over time. Symptoms include shortness of breath, a dry cough, feeling tired, weight loss and nail clubbling. Complications may include pulmonary hypertension, respiratory failure, pneumothorax, and lung cancer.
Pulmonary fibrosis causes include environmental pollution, certain medications, connective tissue diseases, infections (including SARS and SARS-CoV-2 infections), interstitial lung diseases. Idiopathic pulmonary fibrosis (IPF), an interstitial lung disease of unknown cause, is most common. Diagnosis may be based on symptoms, medical imaging, lung biopsy, and lung function tests.
There is no cure and there are limited treatment options available.
Treatment is directed towards efforts to improve symptoms and may include oxygen therapy and pulmonary rehabilitation. Certain medications such as pirfenidone (Esbriet) and nintedanib (Ofev) may be used to try to slow the worsening of scarring. Lung transplantation may occasionally be an option.
At least 6 million people annually are affected globally prior to the COVID-19 pandemic.Life expectancy is generally less than five years. However with the advent of the COVID-19 pandemic, the incidence of pulmonary fibrosis has increased exponentially.
According to the study team, the mitochondrial calcium uniporter (MCU) regulates metabolic reprogramming in lung macrophages and the progression of pulmonary fibrosis. Fibrosis progression is associated with apoptosis resistance in lung macrophages; however, the mechanism(s) by which apoptosis resistance occurs is poorly understood.
The study team found a marked increase in mitochondrial B-cell lymphoma-2 (Bcl-2) in lung macrophages from subjects with idiopathic pulmonary fibrosis (IPF). Similar findings were seen in bleomycin-injured wild-type (WT) mice, whereas Bcl-2 was markedly decreased in mice expressing a dominant-negative mitochondrial calcium uniporter (DN-MCU).
Carnitine palmitoyltransferase 1a (Cpt1a), the rate-limiting enzyme for fatty acid β-oxidation, directly interacted with Bcl-2 by binding to its BH3 domain, which anchored Bcl-2 in the mitochondria to attenuate apoptosis. This interaction was dependent on Cpt1a activity. Lung macrophages from IPF subjects had a direct correlation between CPT1A and Bcl-2, whereas the absence of binding induced apoptosis.
&n
bsp;
Importantly the deletion of Bcl-2 in macrophages protected mice from developing pulmonary fibrosis. Moreover, mice had resolution when Bcl-2 was deleted or was inhibited with ABT-199 after fibrosis was established. These observations implicate an interplay between macrophage fatty acid β-oxidation, apoptosis resistance, and dysregulated fibrotic remodeling.
The breakthrough study findings were published in the peer reviewed journal: Cell Death & Differentiation
https://www.nature.com/articles/s41418-021-00840-w
The research suggests a novel therapeutic target to reverse lung fibrosis.The study team reversed lung fibrosis in a mouse model of idiopathic pulmonary fibrosis, or IPF.
In the study, mice were given bleomycin for 12 days to establish lung fibrosis, and then treated daily until 21 days with ABT-199, whose medical form is known as Venetoclax, a medication approved by the United States Food and Drug Administration for use in several forms of leukemia.
It was found that control bleomycin mice had lung fibrosis with widespread collagen deposition. The bleomycin mice that received ABT-199 had normal lung architecture at 21 days and no collagen deposition.
The study findings suggest a novel therapeutic target to reverse fibrotic remodeling in the lungs, says study leader Dr A. Brent Carter, M.D., professor in the Division of Pulmonary, Allergy and Critical Care Medicine in the University of Alabama at Birmingham Department of Medicine.
The study was also led by first author Dr Linlin Gu, Ph.D., UAB Department of Medicine.
Lung or pulmonary fibrosis is a chronic disease showing aberrant remodeling of lung tissue. Idiopathic pulmonary fibrosis is the most common form of pulmonary fibrosis and has a high mortality rate within three to five years. Currently approved medications have limited efficacy.
The drug ABT-199 acts by inducing apoptosis, or programmed cell death, in monocyte-derived macrophages in the lung. Macrophages are large white blood cells that engulf and digest anything that does not have the surface proteins of healthy cells. Targets can include cancer cells, microbes and cellular debris.
Past studies showed that fibrosis progression was known to be associated with apoptosis resistance in lung macrophages, though the mechanism of that resistance was poorly understood.
Furthermore existing dogma did not point to macrophages as actors in fibrosis; it instead proposed that increased alveolar epithelial cell injury and apoptosis were the initiating events in lung fibrosis.
The cellular activity called apoptosis is a regulated suicide process for cells that are a threat to the organism or are no longer needed. Mitochondria, the organelles that are the powerhouses of the cell, play a key role in the intrinsic pathway of apoptosis.
The study team seeking to better understand the mechanism of how lung macrophages become apoptotic resistant learned that the mitochondria also play a key role in apoptosis resistance.
Utilizing lung lavage, the study team isolated macrophages from individuals with IPF.
The team found a marked increase in the macrophage mitochondrial protein Bcl-2, a regulator of apoptosis as compared to lung macrophages from people without IPF. Mitochondrial Bcl-2 was also elevated in lung macrophages from bleomycin-exposed mice that have lung fibrosis.
Aside from increased Bcl-2 in the mitochondria of lung macrophages from bleomycin mice, the study team also found two proteins: MCU and Cpt1a showed a similar increase in expression.
The MCU protein is a channel to bring calcium into the mitochondria, and Cpt1a is an enzyme in mitochondria that is the rate-limiting step for the fatty acid beta-oxidation energy pathway. MCU was previously known to regulate metabolic reprogramming of lung macrophages to fatty acid oxidation, as well as act in the progression of lung fibrosis and apoptosis resistance.
The study team found that Bcl-2 was regulated by MCU, and that silencing MCU caused a significant decrease for Bcl-2 in the mitochondria of lung macrophages.
The team also found that MCU modulated the binding of Cpt1a to a particular domain of Bcl-2, which anchored Bcl-2 in the mitochondria to attenuate apoptosis. This interaction was dependent on Cpt1a activity.
By studying and looking again at lung macrophages from people with IPF, the team found a direct correlation between the levels of Cpt1a and Bcl-2; the amounts in macrophages from different individuals varied in tandem.
Most significantly the study team found that mice with a conditional deletion of Bcl-2 in lung macrophages were protected from pulmonary fibrosis in the bleomycin model, and they were also protected from asbestos-induced lung fibrosis. These conditional deletion results set the stage for the experiments showing that the Bcl-2 inhibitor ABT-199 was able to reverse fibrosis in the mouse bleomycin model.
Also interestingly ABT-199 completely blocked the Cpt1a-Bcl-2 interaction. In additional genetic evidence, fibrosis was also reversed by the conditional deletion of Bcl-2 in mice with established fibrosis.
Dr Brent Carter, M.D., Professor, Division of Pulmonary, Allergy and Critical Care Medicine, University of Alabama at Birmingham told Thailand Medical News, “The study findings suggest that fatty acid oxidation provokes apoptosis resistance through the stabilization of Bcl-2 in the mitochondria by binding to Cpt1a. Moreover, these data demonstrate that monocyte-derived macrophages are required for fibrosis progression, and they suggest a novel therapeutic target to prevent progressive aberrant fibrotic remodeling."
The study team has already initiated a number of clinical trials that are ongoing and Thailand Medical News will provide updates on these findings.
For more about
Venetoclax and Pulmonary Fibrosis, keep on logging to Thailand Medical News.