Nikhil Prasad Fact checked by:Thailand Medical News Team Jul 04, 2024 9 months, 3 weeks, 22 hours, 52 minutes ago
Long COVID, a condition where COVID-19 symptoms persist for weeks or months after the initial infection, has been a significant challenge for patients and healthcare providers alike. Many individuals experience prolonged fatigue, cognitive issues often referred to as "brain fog," and other debilitating symptoms. Recent research by scientist from University of Wisconsin-Madison, USA and Protibea Therapeutics, Inc-USA that is covered in this
Long COVID News report proposes a promising new treatment to alleviate these neurologic symptoms.
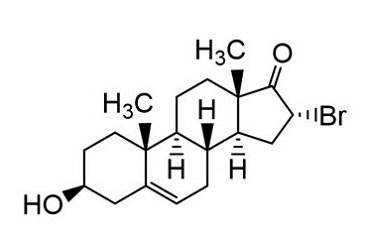
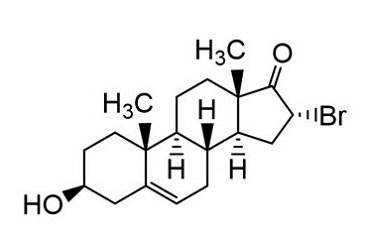 Bromo-Epi-Androsterone (BEA) For Neurologic Long-COVID
Introducing Bromo-Epi-Androsterone (BEA)
Bromo-Epi-Androsterone (BEA) For Neurologic Long-COVID
Introducing Bromo-Epi-Androsterone (BEA)
The study team have suggested that Bromo-Epi-Androsterone (BEA), a synthetic analog of dehydroepiandrosterone (DHEA), as a potential treatment for the neurologic effects of Long COVID. Unlike DHEA, which has androgenic and estrogenic effects, BEA does not produce these hormone-related side effects. This makes BEA a safer option for a broader range of patients.
How BEA Works
BEA works by targeting several mechanisms that contribute to Long COVID. One of its primary actions is to inhibit glucose-6-phosphate dehydrogenase (G6PDH), an enzyme involved in the body's stress response. BEA is about 60 times more potent than DHEA in this role, which helps in reducing inflammation and supporting immune function.
The Connection Between COVID-19 and Brain Health
Long COVID can cause persistent cognitive dysfunction, affecting attention, memory, and executive functioning. This condition, commonly known as brain fog, often accompanies symptoms like fatigue, sleep problems, and loss of smell or taste. Studies indicate that around 22% of COVID-19 patients experience cognitive issues 19 weeks after infection, with some still affected at nine months.
The main driver of these cognitive problems appears to be inflammation triggered by SARS-CoV-2, the virus that causes COVID-19. This inflammation increases the permeability of the blood-brain barrier, activates immune cells in the brain, and can lead to neuronal damage. Chronic inflammation also reduces the brain's ability to generate new neurons and form new connections, further impacting memory and mood.
Immune Dysregulation in Long COVID
SARS-CoV-2 infection triggers the body's immune response to fight off the virus. However, in Long COVID patients, this immune response can become dysregulated. Changes in immune cells, increased levels of autoantibodies (which attack the body's own tissues), and reactivation of dormant viruses like Epstein-Barr contribute to ongoing inflammation and immune dysfunction.
This sustained immune activation produces a range of self-targeting antibodies, which are believed to contribute to various Long COVID symptoms. For instance, high levels of inflammatory cytokines, such as interleukin-6 (IL-6) and interferon-alpha (IFN-α), have been associated with severe Long COVID symptoms, including neurological issues.
The Role of DHEA
and BEA in Immune Health
DHEA and its sulfate form, DHEA-S, are the most abundant steroids in the human body. They play essential roles in metabolism, immune function, and stress response. DHEA levels naturally decline with age, which is associated with increased susceptibility to infections and chronic diseases.
BEA, being a potent analog of DHEA, helps restore immune balance and reduce non-productive inflammation. It supports the immune system by promoting a T1 response, which enhances the body's ability to fight infections and reduces the risk of autoimmune disorders.
Clinical Trials and Future Prospects
Previous formulations of BEA have been tested in clinical trials for various infections, including HIV, malaria, and hepatitis. These trials have shown promising results, leading to the FDA granting investigational new drug status for BEA in treating HIV/AIDS.
Given its broad immune-supporting properties, BEA is now being proposed as a treatment for Long COVID. Researchers believe that by restoring immune homeostasis and reducing inflammation, BEA could significantly improve the neurologic symptoms associated with Long COVID.
Potential Impact on Alzheimer's Disease
Interestingly, the research suggests that studying BEA's effects on Long COVID could also provide insights into its potential benefits for Alzheimer's disease. Both conditions share similar inflammatory pathways and neuroinflammatory biomarkers. By monitoring BEA's impact on Long COVID, scientists hope to gain valuable information about its potential to treat neuroinflammation in Alzheimer's disease.
Conclusion: A Beacon of Hope
As the world continues to grapple with the long-term effects of COVID-19, the proposal of BEA as a treatment for Long COVID brings new hope. By addressing the underlying immune dysregulation and inflammation, BEA has the potential to alleviate the debilitating neurologic symptoms that many Long COVID patients face. If successful, this treatment could also pave the way for new approaches to managing other neuroinflammatory conditions like Alzheimer's disease.
This promising research underscores the importance of continued scientific exploration and clinical trials to find effective treatments for Long COVID and improve the quality of life for millions affected by this condition.
The study findings were published on a preprint server and is currently being peer reviewed.
https://www.preprints.org/manuscript/202407.0115/v1
For the latest
Long COVID News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-causes-glymphatic-drainage-dysfunction-and-bbb-disruption-that-contributes-to-neuroaxonal-injury
https://www.thailandmedical.news/news/covid-19-s-hidden-impact-enlarged-brain-structures-in-some-patients