Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 26, 2024 6 months, 5 hours, 29 minutes ago
Medical News: A recent study has found a strong connection between kidney function indicators and the outcomes of severe COVID-19 cases, especially in patients hospitalized with intense COVID-19 symptoms. The study was conducted by a team of researchers from institutions in Mexico and Bolivia, including the Instituto Nacional de Enfermedades Respiratorias (INER) and Universidad Mayor de San Simón, among others.
 BUN/Cr Ratios Reveal Crucial Link Between Kidney Health and COVID-19 Severity
BUN/Cr Ratios Reveal Crucial Link Between Kidney Health and COVID-19 Severity
This
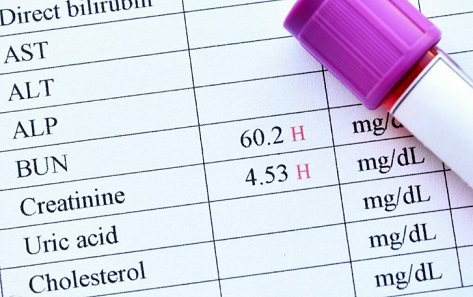
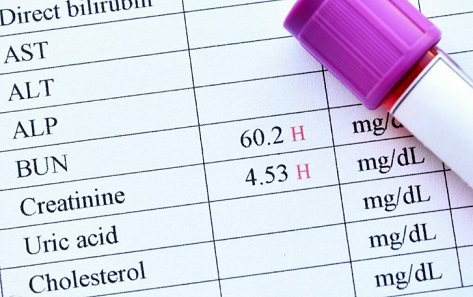
Medical News report delves into the study's key focus: how the blood urea nitrogen to creatinine (BUN/Cr) ratio - a typical marker of kidney function - may reflect not only kidney health but also the severity of COVID-19 in patients. The study followed 3,007 COVID-19 patients over a span of several months and identified correlations between elevated BUN/Cr ratios, acute kidney injury (AKI), and patient outcomes, including mortality.
What is the BUN/Cr Ratio?
The BUN/Cr ratio is a laboratory marker commonly used to measure kidney function. Blood urea nitrogen (BUN) reflects the amount of nitrogen in the blood derived from urea, a byproduct of protein metabolism, while creatinine is a byproduct of muscle metabolism. A high BUN/Cr ratio typically signals prerenal kidney issues, which may arise from dehydration, poor blood flow to the kidneys, or other conditions where the kidneys are strained.
However, researchers have now found that this ratio can indicate more than kidney health in severe COVID-19 cases. In patients with persistent elevation in the BUN/Cr ratio (termed PI-BUN/Cr), there appeared to be increased mortality risk, especially when coupled with AKI.
Study Methodology
The study followed patients admitted to the INER hospital in Mexico City between March 2020 and August 2021. All patients included in the study were confirmed COVID-19 positive through RT-PCR tests. Those with end-stage kidney disease or pre-existing conditions that could interfere with accurate readings of kidney function were excluded. For the majority of patients, researchers used the lowest creatinine levels during hospitalization as a baseline.
Blood urea nitrogen and serum creatinine values were recorded daily, providing a continuous assessment of the patients’ kidney function over time. Other factors considered included age, gender, pre-existing conditions, and whether patients required mechanical ventilation or other intensive treatments.
The Study's Key Findings
Among the 3,007 patients studied, approximately 35% died, with most fatalities occurring in patients who experienced both high BUN/Cr ratios and AKI. Overall, 71.4% of the participants developed AKI during hospitalization, and 44.6% showed persistently high BUN/Cr levels. Importantly, the study grouped patients into categories to better understand how these markers affected survival and kidney function. They found the following:
-Higher Mortality in PI-BUN
/Cr & AKI Patients: Patients who developed both a persistently elevated BUN/Cr ratio and AKI had a significantly higher mortality rate compared to those with only one of these conditions or neither. This finding indicates that the combination of these two kidney-related indicators can be a red flag for severe COVID-19 complications.
-Non-AKI Patients with PI-BUN/Cr also at Risk: Even among patients who did not develop AKI, those with elevated BUN/Cr levels were still at a higher risk of mortality. This suggests that the PI-BUN/Cr metric alone could signal a need for closer monitoring, even if AKI is not present.
-Possible Role of Hyperuricemia in AKI: The study also found that high levels of uric acid (hyperuricemia) correlated with an increased risk of developing AKI in COVID-19 patients. This link indicates that the buildup of uric acid in the body could play a role in damaging kidney function and worsening COVID-19 symptoms.
Implications for COVID-19 Patient Care
The findings of this research point to potential improvements in monitoring and managing COVID-19 in patients with signs of kidney distress. By regularly checking the BUN/Cr ratio, healthcare providers may be able to identify patients at a greater risk of severe illness and mortality early on. This, in turn, could lead to earlier intervention strategies and better outcomes for critically ill patients.
Moreover, the study underscores the importance of kidney health in the context of COVID-19 and highlights the potential for BUN/Cr levels to serve as a predictive tool in managing patient outcomes. By identifying those with a heightened risk of mortality due to AKI or persistently high BUN/Cr ratios, hospitals could adopt targeted treatment strategies to reduce the likelihood of critical complications.
Conclusion
This study sheds new light on the role of kidney function in the progression and severity of COVID-19, with persistently elevated BUN/Cr ratios and the presence of AKI shown to significantly increase the risk of mortality in severe cases. It underscores that ongoing monitoring of kidney function in COVID-19 patients could be crucial to saving lives, as it offers a clearer picture of which patients may require more aggressive or immediate interventions.
The PI-BUN/Cr ratio and its implications on kidney health represent an essential factor in assessing risk, and with further research, it may become an established tool in identifying and managing high-risk patients in various medical settings.
The study findings were published in the peer-reviewed journal: Pneumonia.
https://link.springer.com/article/10.1186/s41479-024-00140-0
For the latest COVID-19 News, keep logging in to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/canadian-study-finds-that-covid-19-causes-unique-endocrine-disruptions
https://www.thailandmedical.news/news/singapore-case-study-reveals-that-even-mild-covid-19-can-trigger-fatal-liver-failure-in-patients-with-autoimmune-liver-disease