Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 23, 2024 1 year, 2 months, 4 days, 10 hours, 20 minutes ago
Medical News: Endocrine Disruptions in COVID-19 Patients: Study Unveils Key Mechanisms and Implications
Researchers from Canada have delved deep into how COVID-19 impacts the endocrine system. The study, conducted by scientists from the Children's Health Research Institute, Lawson Health Research Institute-, and the Department of Pediatrics at Western University, Canada, offers vital insights into how the virus triggers endocrine dysregulation. This
Medical News report explains the mechanisms behind these changes in simpler terms and highlights what this means for treatment and patient care.
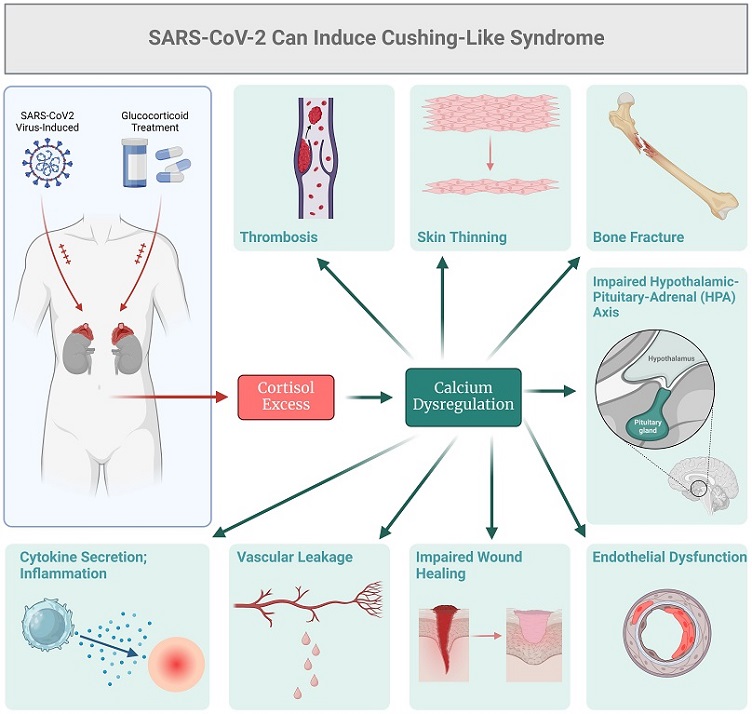
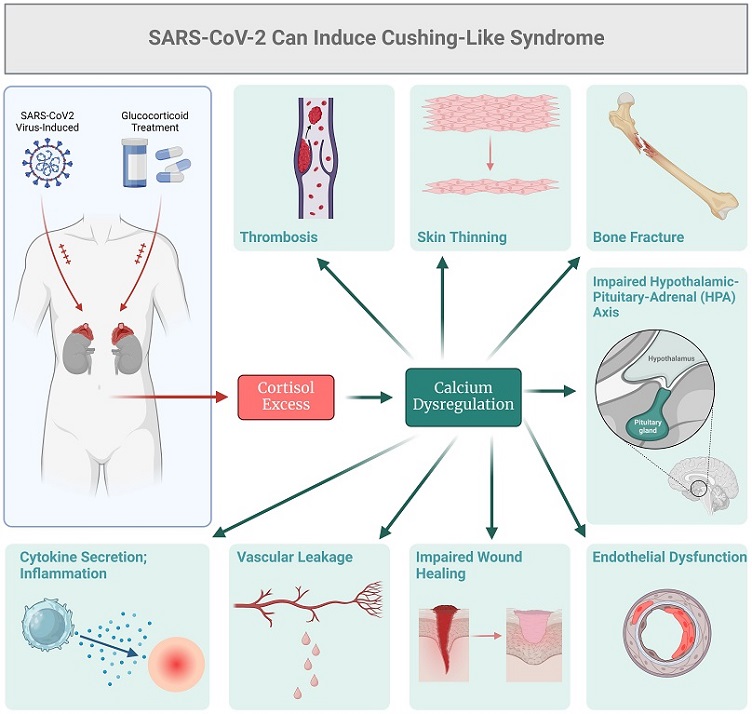 SARS-Cov2 can induce cortisol excess and Cushing's-like syndrome.
A Close Look at COVID-19’s Effect on the Endocrine System
SARS-Cov2 can induce cortisol excess and Cushing's-like syndrome.
A Close Look at COVID-19’s Effect on the Endocrine System
COVID-19 is primarily known for attacking the lungs, but new research is showing it also affects the body’s hormones. The study focuses on how the SARS-CoV-2 virus, which causes COVID-19, disrupts hormone production, particularly cortisol, a hormone produced by the adrenal glands. Cortisol plays a key role in managing stress, inflammation, and immune responses.
Cortisol levels in COVID-19 patients were found to rise due to inflammation and the body’s stress response. Interestingly, this increase in cortisol happens even when the hormone that usually triggers its release - adrenocorticotropic hormone (ACTH) - is not elevated. This phenomenon, often called “pseudo-Cushing’s syndrome,” suggests that COVID-19 may lead to unique endocrine dysfunctions, where the body’s stress system goes into overdrive.
The study highlights that in more severe cases of COVID-19, the virus seems to interfere with not just the cortisol system but other hormonal pathways, leading to a form of “endocrine resistance.” This means the body’s cells stop responding to hormones properly, making it harder for the body to regulate its functions.
The Mechanisms at Play: What Causes Endocrine Dysregulation?
Endocrine dysregulation refers to a situation where hormone-producing glands, such as the adrenal glands, thyroid, or pancreas, do not function properly due to external or internal factors. In COVID-19, researchers discovered that the virus affects these glands in different ways, depending on the severity of the disease.
One major factor is inflammation. The “cytokine storm,” a massive inflammatory response triggered by COVID-19, stimulates the adrenal glands to produce more cortisol. However, sometimes cortisol levels rise even without the presence of ACTH, as the adrenal glands become less responsive to their usual signals. This results in abnormal hormone production.
The study findings also suggest that calcium dysregulation plays a role. Calcium is essential for many bodily functions, including hormone secretion. COVID-19 seems to disrupt calcium signaling pathways, which may further complicate how hormones are produced and regulated.
&
lt;br />
The researchers also observed changes in signaling pathways related to growth factors, such as the insulin-like growth factor (IGF) system. This pathway helps regulate growth, metabolism, and survival of cells. When disrupted, it can lead to conditions resembling endocrine resistance, where cells stop responding to hormonal cues. Such disruptions were particularly noted in severe cases, where IGF signaling was enhanced, making it harder for the body to regulate hormone responses effectively.
Mild vs. Severe Cases: What’s Different?
The study found that the impact of COVID-19 on the endocrine system varies between mild and severe cases. In milder forms of the disease, the body shows an increase in certain proteins like EGFR (epidermal growth factor receptor) and MMP9 (a type of enzyme). These changes can contribute to cell survival and tissue remodeling, which are part of the body’s natural healing process. However, when this process is disrupted, it may lead to what’s known as endocrine resistance, where hormones like cortisol or insulin don’t work as effectively as they should.
On the other hand, in severe cases of COVID-19, more complex disruptions were observed. These involved insulin-like growth factor receptor I (IGF-IR) and the NOTCH signaling pathway, both of which are crucial for cell growth and metabolism. In these cases, patients showed increased levels of survival proteins like Bcl2, along with changes in other proteins involved in stress responses (such as AKT1 and MAPK8). These alterations further worsen endocrine resistance, making the body less responsive to hormone therapy and increasing the severity of the illness.
Potential Therapeutic Implications
The findings from this research point toward new therapeutic approaches for managing COVID-19-related endocrine complications. As endocrine resistance plays a role in worsening disease outcomes, therapies targeting hormone signaling pathways, calcium balance, and growth factors could offer significant benefits.
For example, treatments that modulate the body’s response to growth factors, such as IGF or EGF, may help mitigate the effects of endocrine resistance in severe COVID-19 cases. Additionally, balancing calcium homeostasis could help regulate hormone production and improve overall patient outcomes. The study also hints at potential interventions using EGFR inhibitors, which are currently being explored in clinical trials for COVID-19 treatment.
Conclusion: Why This Matters
The study highlights how COVID-19 doesn’t just attack the lungs but can also disrupt the body’s delicate hormonal balance. This is especially true in severe cases, where the virus interferes with key signaling pathways, leading to a form of endocrine resistance that makes it harder for the body to respond to hormones like cortisol and insulin.
These findings underscore the need for a more comprehensive approach to treating COVID-19, one that takes into account not just the respiratory symptoms but also the broader effects on the endocrine system. By understanding the underlying mechanisms of endocrine disruption, doctors and researchers can develop better-targeted therapies that address both the immediate and long-term effects of the virus.
The study findings were published in the peer-reviewed journal: Frontiers in Endocrinology.
https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1459724/full
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/study-finds-that-covid-19-infections-causes-pancreatic-impairment
https://www.thailandmedical.news/news/viral-infections-including-covid-19-and-thyroid-cancer-a-new-threat-emerges