Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 12, 2025 2 months, 1 day, 7 hours, 22 minutes ago
Medical News: Scientists from the Armand-Frappier Sante Biotechnologie Research Center at the Institut National de la Recherche Scientifique in Laval, Quebec, Canada, have conducted a groundbreaking study on how the immune system responds to COVID-19. Using advanced single-cell transcriptomics, they analyzed bronchoalveolar lavage fluid (BALF) from COVID-19 patients at different severity levels and compared it to healthy individuals. Their findings provide vital insights into why some people experience severe disease while others recover more easily.
 Canadian Study Finds That Immune Dysregulation Drives COVID-19 Severity
Understanding the Immune Changes in Severe COVID-19
Canadian Study Finds That Immune Dysregulation Drives COVID-19 Severity
Understanding the Immune Changes in Severe COVID-19
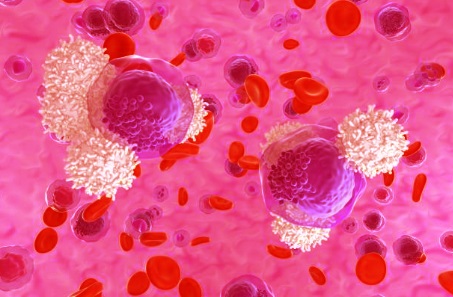
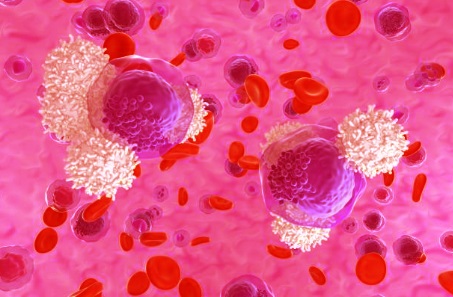
The study revealed that the immune system reacts differently depending on the severity of the disease. This
Medical News report highlights how immune cells like macrophages, neutrophils, T cells, and natural killer (NK) cells behave in severe cases compared to mild infections.
In critically ill patients, macrophages - a type of white blood cell responsible for clearing infections - were found to produce excessive inflammatory proteins, including TNF-alpha and IL1-beta. These pro-inflammatory molecules trigger widespread inflammation and tissue damage in the lungs, worsening the disease.
Neutrophils, another type of immune cell that fights infections, showed prolonged survival in severe cases due to the activation of specific genes such as MCL1 and HIF1-alpha. This led to an increase in the formation of neutrophil extracellular traps (NETs), which are designed to trap and kill pathogens but can also contribute to dangerous blood clots and organ damage in severe COVID-19.
Additionally, macrophages and neutrophils displayed reduced phagocytosis, meaning their ability to engulf and remove harmful substances was impaired. The decreased activity of genes like MSR1, MRC1, and FCGR3B in these cells suggested that dead cells and inflammatory debris were accumulating in the lungs of severe patients, further intensifying inflammation and lung damage.
The Role of T Cells and NK Cells in Disease Severity
The study also uncovered critical dysfunctions in T cells and NK cells, which are essential for fighting infections. In severe COVID-19 cases, T cells showed increased exhaustion, marked by the upregulation of activation markers IFN-gamma and ISG15. This paradoxical activation-exhaustion state weakens the immune response, preventing the body from effectively clearing the virus.
Similarly, NK cells, which play a crucial role in identifying and killing infected cells, exhibited impaired function and reduced numbers in severe cases.
Dendritic cells, which help activate T cells, also appeared to be dysfunctional in severe patients. These cells showed lower expression of key antigen-presenting genes such as HLA-A, HLA-B, and HLA-C, along with a decline in co-stimulatory molecules CD80 and CD86. This suggests that in severe COVID-19, the immune system fails to properly activate and coordinate its defense mechanisms.
&
amp;nbsp;
Implications for Future Treatments
The findings from this study provide valuable insights into potential therapeutic targets for COVID-19. By identifying the immune pathways that contribute to severe disease, researchers can explore new treatments aimed at modulating the immune response. Strategies that could reduce excessive inflammation while preserving the ability to fight the virus may help improve outcomes for patients with severe infections.
Conclusion
This research sheds light on why some individuals develop life-threatening complications from COVID-19 while others experience mild symptoms. The study highlights the crucial role of immune cell dysfunction in disease severity, particularly among neutrophils, macrophages, dendritic cells, and T cells. The insights gained could pave the way for more effective treatments that focus on restoring immune balance and reducing the harmful inflammatory response seen in severe cases. As scientists continue to investigate the complex interactions between the immune system and SARS-CoV-2, the hope is to develop better strategies to manage and treat COVID-19 effectively.
The study findings were published in the peer-reviewed journal: PLOS ONE.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0309880
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/groundbreaking-study-offers-insight-into-the-long-term-immune-effects-of-covid-19
https://www.thailandmedical.news/news/how-viral-rna-triggers-immune-overdrive-and-suppressed-antiviral-defenses
https://www.thailandmedical.news/news/covid-19-poses-long-term-risks-for-autoimmune-disorders
https://www.thailandmedical.news/articles/coronavirus