Cefiderocol : New antibiotic effective against drug-resistant bacteria in phase 2 trial
Source: Lancet Nov 01, 2018 6 years, 5 months, 3 weeks, 5 days, 2 hours, 27 minutes ago
Results from a phase 2 randomised trial suggest that a new investigational antibiotic is as effective as the current standard-of-care antibiotic for the treatment of complicated urinary tract infections (UTIs) caused by several multidrug resistant Gram-negative bacteria.
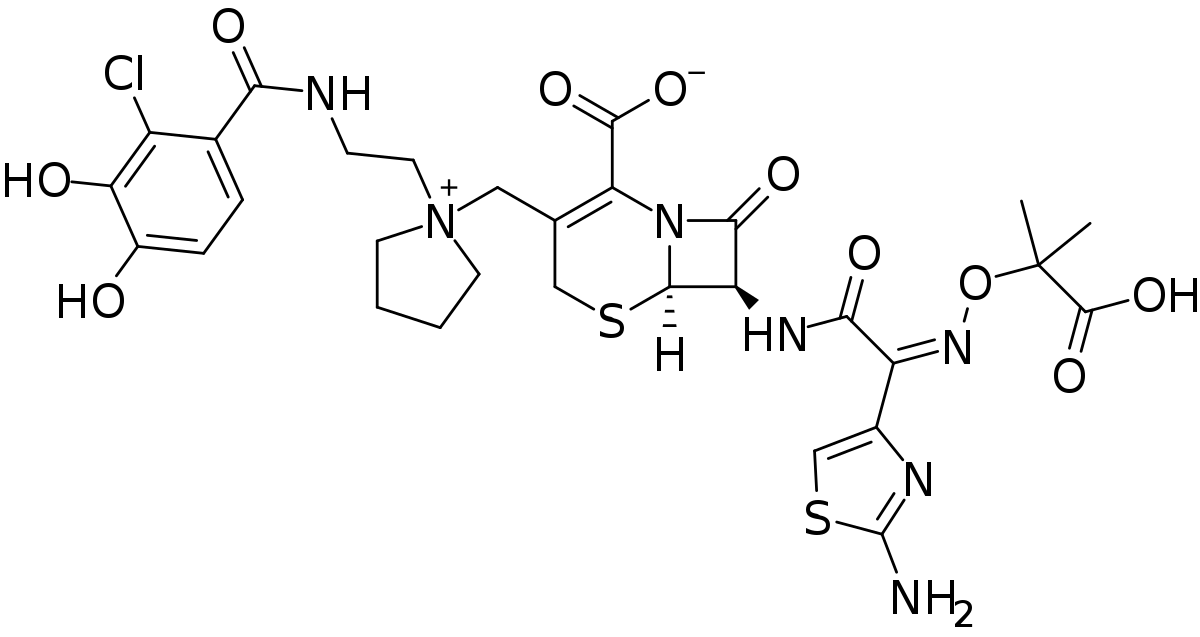
The findings, published in The Lancet Infectious Diseases, indicated that patients treated with the siderophore-based drug, cefiderocol, had a higher and more sustained level of pathogen eradication and similar clinical outcomes to those treated with the current standard of care, imipenem-cilastatin.
Cefiderocol is novel in its approach to overcoming the three main mechanisms of antibiotic resistance used by Gram-negative bacteria -- two outer membranes that make it hard for antibiotics to penetrate, porin channels which can adapt and change to block the antibiotic entry, and efflux pumps that expel antibiotics back out of the cell and
make the drugs ineffective.
"Cefiderocol acts as a trojan horse," explains Dr Simon Portsmouth, Shionogi Inc, USA, who led the research. "The drug uses a novel mechanism of cell entry that takes advantage of the bacteria's need for iron to survive. During an acute infection, one of our innate immune responses is to create an iron-poor environment. In response, bacteria increase their iron intake. Cefiderocol binds to irons and is transported through the extra outer membrane by the bacterium's own iron-transport system. These iron channels also enable the drug to bypass the bacteria's porin channels and gain repeat entry even if the bacterium has evolved efflux pumps."
The findings highlight the potential of cefiderocol as an important new option for treating highly resistant Gram-negative bacteria, once approved. Cefiderocol's effect on carbapenem-resistant strains -- which cause some of the hardest-to-treat infections in
health-care settings, and for which there is no antibiotic alternative that does not have serious side effects or other complications -- could not be properly evaluated because the carbapenem drug imipenem-cilastatin was used as the active control treatment.
The US Centers for Disease Control and Prevention (CDC) estimate that antibiotic-resistant microorganisms cause more than two million infections in the USA each year, resulting in at least 23,000 deaths. A 2014 Review on Antimicrobial Resistance predicted that by 2050, the global cost of antibiotic resistance will rise to as such as £100 trillion and account for 10 million deaths every year.
Antibiotic resistance has been identified as one of the biggest threats to human health globally. While the antibiotic arsenal dwindles in effectiveness, new antibiotics with novel modes of action are urgently needed. WHO considers carbapenem-resistant, Gram-negative pathogens including Pseudomonas aeruginosa, Acinetobacter baumannii, and Enterobacteriaceae as the highest priority and critical for development of new antibiotics. Previous studies have demonstrated that cefiderocol is active against all three multidrug-resistant pathogens.
As part of the US Food and Drug Administration (FDA) approach to fast-tracking antibiotic development, this study randomised 448 adults (aged 18 or older) who had been hospitalised with a complicated UTI or uncomplicated pyelonephritis (inflammation of the kidney dur
to a bacterial infection) to receive three daily infusions of cefiderocol (300 patients) or imipenem-cilastatin (148 patients) for seven to 14 days. In total, 252 patients treated with cefiderocol and 119 with imipenem-cilastatin had a Gram-negative uropathogen and were included in the efficacy analysis. The majority of participants had Escherichia coli, Klebsiella pneumoniae, or P aeruginosa infections.
Results suggested that cefiderocol was as effective as imipenem-cilastatin in a combined evaluation of the clinical and microbiological response with efficacy rates of 73% (183/252 patients) and 55% (65/119 patients) respectively seven days after treatment was stopped. This difference was mainly driven by the sustained antibacterial activity of cefiderocol whilst the clinical responses were highly similar (90% vs 87%).
Overall, cefiderocol was well tolerated with similar numbers of adverse events to that of imipenem-cilastatin (41% [122/300 patients] vs 51% [76/148 patients]). Gastrointestinal disorders (ie, diarrhea, constipation, nausea, vomiting, and abdominal pain) were the most common adverse events in both groups (35 [12%] patients in the cefiderocol group and 27 [18%] patients in the imipenem-cilastatin group). Fourteen (5%) participants in the cefiderocol group and 12 (8%) in the imipenem-cilastatin group reported at least one serious adverse event, with C difficile colitis the most common.
Dr Portsmouth says: "Cefiderocol was found to be both safe and tolerable in a population of older patients who were very ill with complex comorbid conditions and a wide range of multidrug-resistant pathogens. Our results support cefiderocol as a novel approach that might be used to overcome Gram-negative resistance."
"Ongoing clinical trials of pneumonia, including hospital-acquired pneumonia and ventilator-associated pneumonia, and a study in patients with carbapenem-resistant infections, will provide additional important information about cefiderocol."
The authors note that an important limitation of the study was the exclusion of patients with carbapenem-resistant infections because the comparator was a carbapenem.
Writing in a linked Comment, Dr Angela Huttner, Geneva University Hospitals, Switzerland, discusses the importance of assessing the post-market clinical experience of the drug: "The FDA's new guidance on complicated urinary tract infection endpoints, issued in June 2018, calls for complete clinical resolution and changed the cutoff for microbiological response to bacterial counts of less than 1 × 103 CFU/mL. An accelerated process to get new antibiotics to market was urgently needed, and regulatory bodies responded. But any trial launched more than four months ago (including an ongoing phase 3 cefiderocol trial, NCT02714595) will now be adhering to outdated standards and requirements. There is still no guidance on measuring baseline or emerging resistance; this too will fall to post-market development. Although these results are promising with regard to obtaining approval for cefiderocol and in the context of increasing antimicrobial resistance, scepticism will persist until more evidence is available. Cefiderocol remains on the fast track to approval. This is welcome news, as long as those in post-market clinical medicine understand the deal we have made: it will fall to us to continue the drug's clinical development, while managing its appropriate use and conservation, and thus take its true measure."
Reference: Simon Portsmouth, David van Veenhuyzen, Roger Echols, Mitsuaki Machida, Juan Camilo Arjona Ferreira, Mari Ariyasu, Peter Tenke, Tsutae Den Nagata. Cefiderocol versus imipenem-cilastatin for the treatment of complicated urinary tract infections caused by Gram-negative uropathogens: a phase 2, randomised, double-blind, non-inferiority trial. The Lancet Infectious Diseases, 2018; DOI: 10.1016/S1473-3099(18)30554-1