Chronic intestinal failure - Advances in management, treatment and real-life challenges
Nikhil Prasad Fact checked by:Thailand Medical News Team Aug 11, 2024 8 months, 2 weeks, 1 day, 14 hours, 31 minutes ago
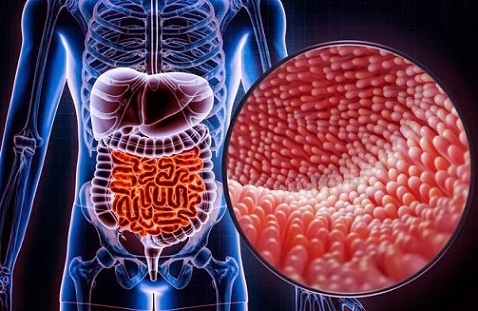
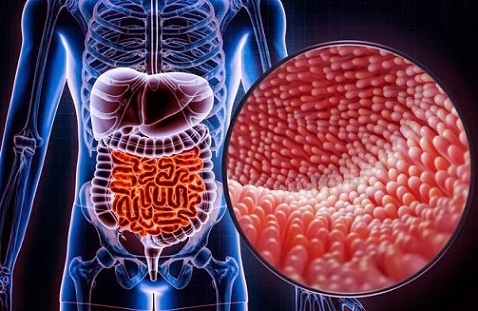
Gastroenterology Updates: Chronic Intestinal Failure (CIF) is a severe and complex condition that affects individuals worldwide, necessitating intricate, multidisciplinary care. This condition is not limited to a particular age group, impacting both children and adults. CIF arises when the intestine's ability to absorb essential nutrients, water, and electrolytes falls below the minimum necessary levels, often requiring patients to rely on parenteral nutrition (PN) or intravenous fluid and electrolytes (IVFEs) to maintain their health and well-being. This
Gastroenterology Updates news report delves into the current status of CIF management, highlighting the gap between ideal management recommendations and real-life practices, particularly in low-income countries.
 Chronic intestinal failure - Advances in management, treatment and real-life challenges
Understanding Chronic Intestinal Failure
Chronic intestinal failure - Advances in management, treatment and real-life challenges
Understanding Chronic Intestinal Failure
CIF is characterized by the need for long-term intravenous supplementation due to the intestine's inability to sustain normal nutrition and hydration. The most common cause of CIF is Short Bowel Syndrome (SBS), where significant portions of the small intestine are either missing or non-functional. Other causes include intestinal dysmotility, extensive small bowel mucosal disease, and chronic intestinal pseudo-obstruction (CIPO). The management of CIF is complex, requiring specialized care teams and a multifaceted approach that includes surgical intervention, medical management, and nutritional support.
Ideal Management vs. Real-Life Management
The management of CIF should ideally follow a structured approach, incorporating the latest advancements in medical science and surgical techniques. However, there is often a significant gap between what is recommended in guidelines and what is practically applied, especially in resource-limited settings. This article highlights these disparities, emphasizing the need for global cooperation to ensure that all patients have access to comprehensive CIF treatment.
Ideal Management Approach
In an ideal scenario, CIF management would be tailored to the individual's specific condition and involve a multidisciplinary team (MDT) of experts. This team should be capable of offering intravenous supplementation in acute and chronic conditions, performing complex abdominal surgeries, and managing CIF patients and transplant cases. The MDT should also include specialists in nutrition, psychology, and physical rehabilitation, ensuring that all aspects of the patient's well-being are addressed.
-Home Intravenous Supplementation (HIVS): This is the cornerstone of CIF management, allowing patients to receive necessary nutrients and fluids at home, reducing hospital stays, and improving their quality of life. HIVS programs must be managed by an experienced MDT to minimize complications such as catheter-related infections and liver disease.
-Surgical Interventions: Surgery is often nece
ssary to improve the anatomy of the intestine, increase its absorptive capacity, or restore continuity. Procedures such as autologous gastrointestinal reconstruction surgery (AGIRS) and serial transverse enteroplasty (STEP) are employed to achieve these goals. The timing of surgery is critical, and it should only be performed when the patient's nutritional status has been optimized.
-Medical Management: Medical treatment involves the use of drugs to manage symptoms and complications. Antimotility agents like loperamide and codeine, along with antisecretory drugs such as proton-pump inhibitors (PPIs), are commonly used. In cases of SBS, the use of semisynthetic glucagon-like peptide-2 (sGLP-2) analogues, such as teduglutide, has shown promise in improving intestinal function and reducing the need for HIVS.
-Nutritional Support: Nutritional management is individualized based on the patient's anatomy and the extent of their intestinal function. The primary goal is to promote intestinal adaptation, a process that can take years. Diets are tailored to include nutrients that stimulate intestinal growth and function while avoiding foods that exacerbate symptoms.
Real-Life Challenges
Despite the advancements in CIF management, many patients around the world do not have access to these ideal treatments. The reality of managing CIF is often constrained by the availability of resources, trained professionals, and infrastructure. In many countries, CIF is still poorly understood, and specialized care teams are scarce. As a result, patients often receive suboptimal care, leading to poor outcomes.
-Access to HIVS: In many low- and middle-income countries, the development of HIVS programs has been limited. Even in countries where such programs exist, the quality of care can vary significantly. For instance, in Europe and the United States, HIVS is often provided by specialized home care companies, while in other regions, local pharmacies or hospitals may handle it, leading to inconsistencies in care.
-Surgical Expertise: The availability of skilled surgeons who can perform complex CIF-related procedures is another significant challenge. In many regions, there are few surgeons with the expertise to perform AGIRS or STEP, leading to delays in treatment and poorer outcomes. Furthermore, the lack of training programs and recognition of intestinal failure and transplant surgery as a subspecialty further exacerbates this issue.
-Medical and Nutritional Management: The use of advanced medical treatments like sGLP-2 analogues is often limited by cost and availability. In many parts of the world, these treatments are not accessible, and patients must rely on less effective therapies. Nutritional management also varies widely, with some patients receiving inadequate dietary guidance due to a lack of trained dietitians.
The Need for Global Cooperation
To bridge the gap between ideal and real-life management of CIF, there is a pressing need for international cooperation and the development of global networks. These networks would facilitate the sharing of expertise, resources, and best practices, ensuring that patients in all regions have access to the care they need. Additionally, there is a need for greater awareness and education about CIF among healthcare professionals, particularly in low-resource settings.
Conclusion
Chronic Intestinal Failure is a complex and debilitating condition that requires a multidisciplinary approach to manage effectively. While significant advancements have been made in the treatment of CIF, there is still a substantial gap between ideal management practices and the reality faced by many patients worldwide. Addressing these disparities requires a concerted effort from the global medical community to ensure that all patients, regardless of their location, have access to the best possible care.
The study findings were published in the peer-reviewed journal: Nutrients.
https://www.mdpi.com/2072-6643/16/16/2648
For the latest
Gastroenterology Updates, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/probiotic-lactobacillus-acidophilus-protects-the-intestines-from-inflammation
https://www.thailandmedical.news/news/covid-19-news-emerging-studies-shows-sars-cov-2-attacks-the-digestive-tract-especially-the-intestines-directly,-reported-case-of-bowel-perforation