Coronavirus News: U.S. NIH Autopsy Studies Shows Severe Brain Damage In COVID-19 Patients
Source: Coronavirus News Jan 02, 2021 4 years, 3 months, 3 weeks, 3 days, 6 hours, 37 minutes ago
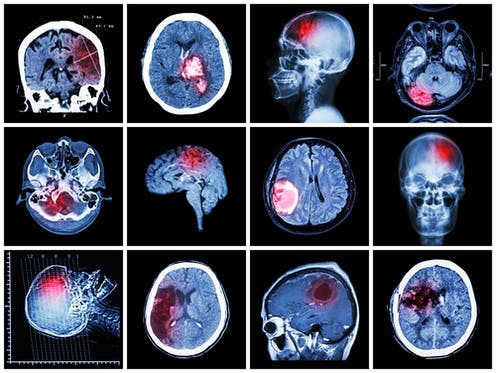
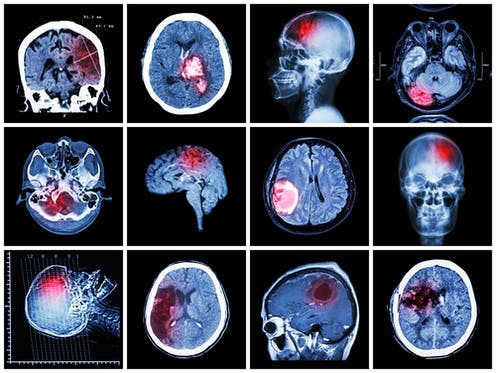
Coronavirus News: A detailed autopsy study conducted by the U.S. National Institutes of Health has alarmingly uncovered hallmarks of damage caused by thinning and leaky brain blood vessels in tissue samples from COVID-19 patients who died shortly after contracting the disease.
However, the researchers saw no signs of SARS-CoV-2 in the tissue samples, suggesting the damage was not caused by a direct viral attack on the brain.
The study team conducted postmortem high-resolution magnetic resonance imaging (magnetic resonance microscopy) of the brains of patients with COVID-19) (median age, 50 years) and histopathological examination that focused on microvascular changes in the olfactory bulb and brain stem. Images were obtained from the brains of 13 patients with the use of an 11.7-Tesla scanner at a resolution of 25 μm for the olfactory bulb and at a resolution of 100 μm for the brain. Abnormalities were seen in the brains of 10 patients.
The study team examined the brains of patients that showed abnormalities by means of multiplex fluorescence imaging (in 5 patients) and by means of chromogenic immunostaining (in 10 patients).
The study team also performed conventional histopathological examination of the brains of 18 patients. Fourteen patients had chronic illnesses, including diabetes and hypertension, and 11 had been found dead or had died suddenly and unexpectedly. Of the 16 patients with available medical histories, 1 had delirium, 5 had mild respiratory symptoms, 4 had acute respiratory distress syndrome, 2 had pulmonary embolism, and the symptoms were not known in 3.
Magnetic resonance microscopy showed punctate hyperintensities in 9 patients, which represented areas of microvascular injury and fibrinogen leakage. These features were observed on corresponding histopathological examination performed with the use of fluorescence imaging. These areas showed thinning of the basal lamina of the endothelial cells, as determined by collagen IV immunostaining in 5 patients. Punctate hypointensities on imaging in 10 patients corresponded to congested blood vessels with surrounding areas of fibrinogen leakage and relatively intact vasculature. Areas of linear hypointensities were interpreted as microhemorrhages . There was minimal perivascular inflammation in the specimens examined, but there was no vascular occlusion.
Perivascular-activated microglia, macrophage infiltrates, and hypertrophic astrocytes were seen in 13 patients. There were CD3+ and CD8+ T cells in the perivascular spaces and in lumens adjacent to endothelial cells in 8 patients, which may have contributed to vascular injury, as suggested in a previous report. Activated microglia were found adjacent to neurons in 5 patients, which is suggestive of neuronophagia in the olfactory bulb, substantia nigra, dorsal motor nucleus of the vagal nerve, and the pre-Bötzinger complex in the medulla, which is involved in the generation of spontaneous rhythmic breathing.
SARS-CoV-2 was not detected by means of polymerase chain reaction with multiple primer sets, RNA sequencing of several areas of the brain, or RNA in situ hybridization and immunostaining. It is possible that the virus was cleared by the time of death or that viral copy numbers were below the level of detection by the assays.
In a convenience sample of patients who had died fr
om COVID-19, multifocal microvascular injury was observed in the brain and olfactory bulbs by means of magnetic resonance microscopy, histopathological evaluation, and immunohistochemical analysis of corresponding sections, without evidence of viral infection.
These study findings may inform the interpretation of changes observed on magnetic resonance imaging of punctate hyperintensities and linear hypointensities in patients with COVID-19. Because of the limited clinical information that was available, no conclusions can be drawn in relation to neurologic features of COVID-19.
The study findings were published as a correspondence in the New England Journal of Medicine.
https://www.nejm.org/doi/10.1056/NEJMc2033369
Dr Avindra Nath, M.D., clinical director at the NIH's National Institute of Neurological Disorders and Stroke (NINDS) and the senior author of the study told Thailand Medical News, "We found that the brains of patients who contract infection from SARS-CoV-2 may be susceptible to microvascular blood vessel damage. Our results suggest that this may be caused by the body's inflammatory response to the virus. We hope these results will help doctors understand the full spectrum of problems patients may suffer so that we can come up with better treatments."
Despite COVID-19 being primarily a respiratory disease, patients often experience neurological problems including headaches, delirium, cognitive dysfunction, dizziness, fatigue, and loss of the sense of smell. The disease may also cause patients to suffer strokes and other neuropathologies. Several studies have shown that the disease can cause inflammation and blood vessel damage. In one of these studies, the researchers found evidence of small amounts of SARS-CoV-2 in some patients' brains. Nevertheless, scientists are still trying to understand how the disease affects the brain.
The study conducted an in-depth examination of brain tissue samples from 19 patients who had died after experiencing COVID-19 between March and July 2020. Samples from 16 of the patients were provided by the Office of the Chief Medical Examiner in New York City while the other 3 cases were provided by the department of pathology at the University of Iowa College of Medicine, Iowa City. The patients died at a wide range of ages, from 5 to 73 years old.
These COVID-19 patients died within a few hours to two months after reporting symptoms. Many patients had one or more risk factors, including diabetes, obesity, and cardiovascular disease. Eight of the patients were found dead at home or in public settings. Another three patients collapsed and died suddenly.
The study team used a special, high-powered magnetic resonance imaging (MRI) scanner that is 4 to 10 times more sensitive than most MRI scanners, to examine samples of the olfactory bulbs and brainstems from each patient. These regions are thought to be highly susceptible to COVID-19.
It must be noted that the olfactory bulbs control our sense of smell while the brainstem controls our breathing and heart rate. The scans revealed that both regions had an abundance of bright spots, called hyperintensities, that often indicate inflammation, and dark spots, called hypointensities, that represent bleeding.
The study team then used the scans as a guide to examine the spots more closely under a microscope. They found that the bright spots contained blood vessels that were thinner than normal and sometimes leaking blood proteins, like fibrinogen, into the brain. This appeared to trigger an immune reaction.
These spots were surrounded by T cells from the blood and the brain's own immune cells called microglia. In contrast, the dark spots contained both clotted and leaky blood vessels but no immune response.
Dr Nath added, "We were completely surprised. Originally, we expected to see damage that is caused by a lack of oxygen. Instead, we saw multifocal areas of damage that is usually associated with strokes and neuroinflammatory diseases."
Importantly the researchers saw no signs of infection in the brain tissue samples even though they used several methods for detecting genetic material or proteins from SARS-CoV-2.
Dr Nath concluded, "So far, our results suggest that the damage we saw may not have been not caused by the SARS-CoV-2 virus directly infecting the brain. In the future, we plan to study how COVID-19 harms the brain's blood vessels and whether that produces some of the short- and long-term symptoms we see in patients."
For more
Coronavirus-19 News, keep on logging to Thailand Medical News.