Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 11, 2024 10 months, 5 days, 6 hours, 30 minutes ago
Medical News: COVID-19, the virus that changed the course of global health, is now revealing its long-term impact on survivors. Beyond the immediate respiratory symptoms, scientists are uncovering alarming connections between the virus and accelerated aging in the brain and immune system. A pivotal study by Ludmila Müller and Svetlana Di Benedetto of the Max Planck Institute for Human Development in Berlin provides insights into how COVID-19 induces processes akin to aging. Their findings underscore the urgent need to address these consequences for global health.
 COVID-19 Accelerates Brain and Immune Aging
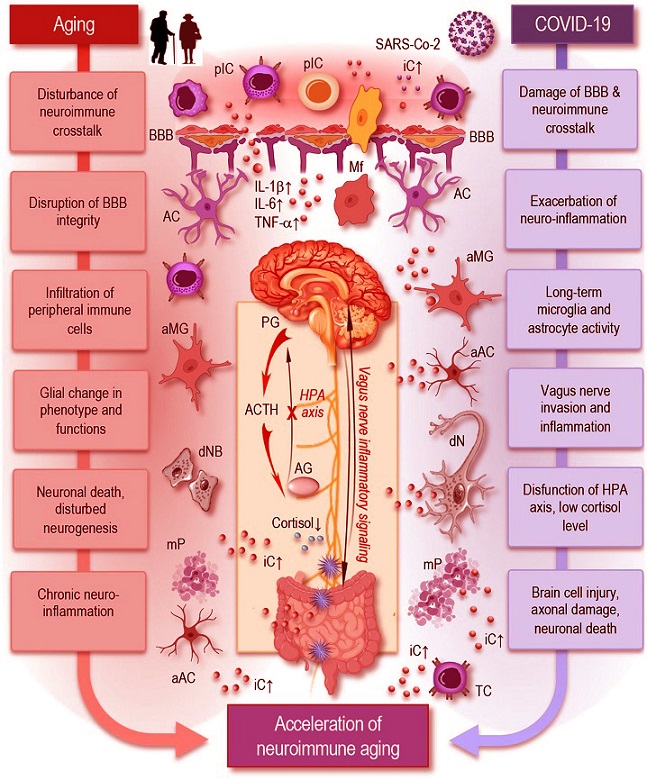
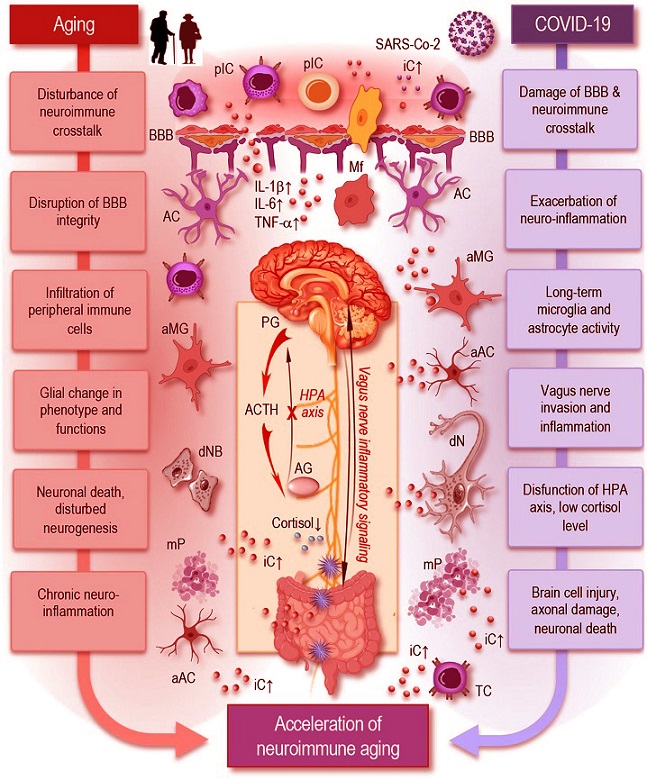
Aging and COVID-19 share significant overlaps in their impact on neuroimmune interactions and may accelerate neuroimmune aging. As depicted in this simplified figure, both aging and COVID-19 can induce neuroinflammation through the accumulation of senescent cells, persistent microglia and astrocytes’ activation, and increased pro-inflammatory cytokine production, such as IL-1β, IL-6, and TNF-α. Similar to aging, SARS-CoV-2 infection can cause significant damage to the blood–brain barrier, facilitating the infiltration of peripheral immune cells and inflammatory mediators into the brain, which disrupts neuroimmune crosstalk and accelerates neuroimmune aging. Inflammatory signaling via the vagus nerve exacerbates neuroinflammatory responses, potentially influencing systemic inflammation and immune responses. The HPA axis experiences dysfunction, resulting in decreased cortisol levels, further exacerbating neuroinflammation. These factors create a chronic inflammatory environment that can damage neurons, disrupt synaptic connectivity, and impair neuroimmune interactions leading to accelerated neuroimmune aging.
The Emerging Crisis of Long COVID
COVID-19 Accelerates Brain and Immune Aging
Aging and COVID-19 share significant overlaps in their impact on neuroimmune interactions and may accelerate neuroimmune aging. As depicted in this simplified figure, both aging and COVID-19 can induce neuroinflammation through the accumulation of senescent cells, persistent microglia and astrocytes’ activation, and increased pro-inflammatory cytokine production, such as IL-1β, IL-6, and TNF-α. Similar to aging, SARS-CoV-2 infection can cause significant damage to the blood–brain barrier, facilitating the infiltration of peripheral immune cells and inflammatory mediators into the brain, which disrupts neuroimmune crosstalk and accelerates neuroimmune aging. Inflammatory signaling via the vagus nerve exacerbates neuroinflammatory responses, potentially influencing systemic inflammation and immune responses. The HPA axis experiences dysfunction, resulting in decreased cortisol levels, further exacerbating neuroinflammation. These factors create a chronic inflammatory environment that can damage neurons, disrupt synaptic connectivity, and impair neuroimmune interactions leading to accelerated neuroimmune aging.
The Emerging Crisis of Long COVID
While the acute phase of COVID-19 gained attention for its high morbidity and mortality, researchers are now shifting focus to long COVID - a condition affecting 1 in 5 survivors. Characterized by symptoms like fatigue, cognitive dysfunction, and respiratory issues, long COVID has become a significant public health concern. This
Medical News report explores how the virus interacts with the aging process, creating new challenges for healthcare systems worldwide.
How COVID-19 Mimics and Accelerates Aging
COVID-19 induces a cascade of effects on the body, particularly on the immune and nervous systems. The study highlights several mechanisms through which the virus accelerates aging:
-Chronic Inflammation as a Catalyst: Known as inflammaging, this persistent low-grade inflammation is common in aging. COVID-19 exacerbates this state by triggering cytokine storms, leading to elevated levels of inflammatory markers such as IL-6, TNF-α, and IL-1β. These markers disrupt cellular processes and impair immune regulation, paving the way for long-term health issues.
-Immune System Decline: Aging naturally weakens the immune system - a proces
s called immunosenescence. COVID-19 worsens this by depleting naïve immune cells and increasing senescent cells, which are less effective in fighting infections and more likely to cause inflammation.
-Neuroinflammation and Cognitive Decline: The virus penetrates the central nervous system, causing neuroinflammation. This damages neurons and disrupts brain function, leading to memory loss, attention deficits, and impaired decision-making in survivors. Studies show that these effects can persist for months or even years.
-Reactivation of Latent Viruses: Long COVID often involves the reactivation of dormant viruses like Epstein-Barr virus (EBV) and cytomegalovirus (CMV). This adds another layer of immune system stress, contributing to prolonged symptoms and greater susceptibility to other illnesses.
-Impact on All Age Groups: Although older adults are more vulnerable due to pre-existing immunosenescence, younger populations are not immune. Even individuals in their 30s and 40s experience persistent cognitive challenges, highlighting the widespread reach of long COVID.
Detailed Findings from the Study
The study reveals several alarming trends:
-Long-Term Cognitive Impairments: Survivors across all age groups report difficulties with memory, executive function, and attention. For some, these impairments resemble conditions typically seen in aging, such as dementia.
-Accelerated Neuroimmune Aging: The virus amplifies neuroimmune interactions, creating a feedback loop of inflammation and neural damage. This interplay increases the risk of neurodegenerative diseases like Alzheimer’s and Parkinson’s.
-Biological Markers of Damage: Elevated levels of markers like neurofilament light chain (NFL) and glial fibrillary acidic protein (GFAP) in COVID-19 patients indicate ongoing brain injury. These markers are typically associated with aging and neurodegenerative diseases.
-Gut-Brain Axis Disruption: COVID-19 affects gut health, leading to dysbiosis - a harmful imbalance in gut microbiota. This, in turn, exacerbates systemic inflammation and neuroinflammation, further impairing cognitive function.
Implications for Public Health
The widespread impact of long COVID has profound implications for healthcare systems. The condition not only affects individuals’ quality of life but also increases the burden on medical infrastructure. As more people live with persistent symptoms, there is a growing need for specialized care and targeted therapies.
Exploring Potential Interventions
To combat the effects of COVID-19 on aging, the researchers suggest a multi-pronged approach:
-Anti-Inflammatory Therapies: Medications targeting inflammation, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids, may help reduce long-term damage.
-Immunomodulatory Treatments: Therapies that restore immune balance, such as cytokine inhibitors and immune checkpoint inhibitors, could mitigate the effects of immunosenescence.
-Neuroprotective Agents: Antioxidants and drugs enhancing synaptic plasticity may preserve brain health and prevent neurodegeneration in COVID-19 survivors.
-Lifestyle Changes: Regular exercise, a nutrient-rich diet, and stress management techniques like mindfulness can promote overall health and resilience against long-term effects.
-Targeting the Gut Microbiome: Improving gut health through prebiotics, probiotics, and dietary changes could reduce inflammation and support immune function.
-Advanced Therapies: Emerging treatments like senolytics, which target and eliminate senescent cells, hold promise for reversing some effects of aging accelerated by COVID-19.
Concluding Insights
The findings of this study underscore the urgent need to address the long-term impacts of COVID-19. The virus accelerates processes of aging in both the immune and nervous systems, creating challenges that will persist long after the pandemic subsides. By investing in research and developing targeted therapies, we can improve outcomes for millions of survivors and reduce the broader societal burden.
Final Thoughts
The fight against COVID-19 is far from over. As we learn more about its long-term effects, it becomes increasingly clear that addressing these challenges requires a coordinated, multidisciplinary approach. From understanding the underlying mechanisms of accelerated aging to implementing effective interventions, there is much work to be done.
The study findings were published in the peer-reviewed journal: Frontiers in Cellular Neuroscience.
https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2024.1471192/full
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/sars-cov-2-spike-protein-accelerates-aging-of-blood-vessels
https://www.thailandmedical.news/news/covid-19-accelerates-biological-aging