Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 26, 2024 1 year, 11 months, 1 day, 4 hours, 39 minutes ago
COVID-19 News: Amid the global COVID-19 pandemic, medical communities worldwide are grappling with an array of challenges posed by the novel coronavirus, SARS-CoV-2. Beyond its primary respiratory manifestations, mounting evidence suggests that COVID-19 may have far-reaching effects, including potential associations with autoimmune conditions such as Adult-Onset Still's Disease (AOSD). AOSD, though rare, presents a complex clinical picture characterized by systemic inflammation, recurrent fevers, arthritis, and distinctive rashes. This
COVID-19 News report aims to explore the intriguing interplay between COVID-19 and AOSD, shedding light on shared pathophysiological pathways and clinical implications based on cases studies by researchers from Brown University-USA and Universidad Colegio Mayor de Nuestra Señora del Rosario-Colombia.
 COVID-19 Can Cause New Adult-Onset Still’s Disease (AOSD)
COVID-19 Can Cause New Adult-Onset Still’s Disease (AOSD)
A number of previous studies and cases reports also validated that SARS-CoV-2 infections can cause Adult-Onset Still’s Disease.
https://ojrd.biomedcentral.com/articles/10.1186/s13023-023-02651-3
https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913%2821%2900072-2/fulltext
https://journals.sagepub.com/doi/10.1177/11795441231161640
https://onlinelibrary.wiley.com/doi/full/10.1002/ccr3.7006
https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/en/covidwho-1405604
https://journals.lww.com/md-journal/fulltext/2022/10070/covid_19_in_a_patient_with_new_adult_onset_still.114.aspx
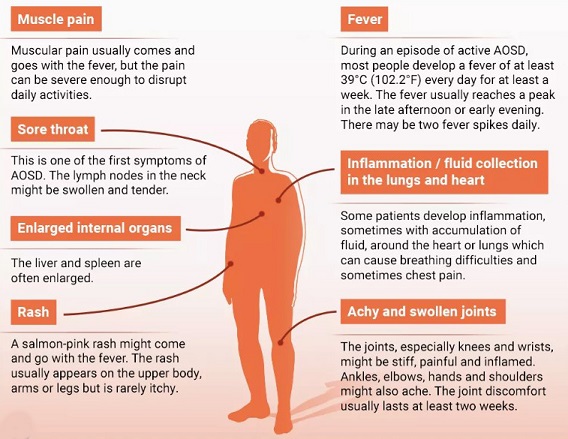
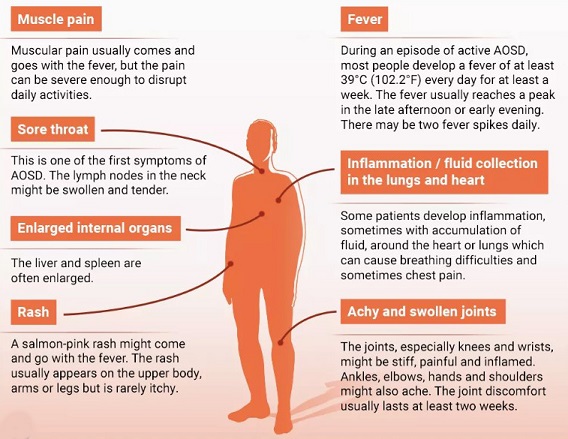
Thailand
Medical News would also like to add that with the advent of the JN.1 variant and its new sub-lineages, the incidences of many individuals developing a milder phenotype of New Adult-Onset Still’s Disease is rampant i.e. most developing light chills or light fevers, sore throats along with accompanying body pains and a smaller number of the distinctive rashes appearing on the lower limbs. Most of these attacks are aggravated after going outdoors in crowded settings and most people above the age of 40 are predominantly affected. Swollen lymph nodes are also often seen.
Understanding Adult-Onset Still's Disease (AOSD)
AOSD
remains an enigmatic entity in the realm of autoimmune disorders. Characterized by its hallmark features of persistent fever, arthritis, and salmon-pink rash, AOSD poses diagnostic challenges due to its overlapping clinical presentation with various infectious and rheumatological conditions. Diagnosis often involves exclusion, relying on a combination of clinical criteria, including fever, arthritis, rash, and laboratory abnormalities such as leukocytosis and elevated acute-phase reactants.
The COVID-19 Conundrum
As the COVID-19 pandemic unfolds, clinicians worldwide have observed diverse clinical presentations, ranging from mild respiratory illness to severe multiorgan dysfunction. Beyond its primary respiratory effects, COVID-19 has been implicated in a spectrum of extrapulmonary manifestations, including neurological, cardiovascular, and autoimmune phenomena. Studies have reported associations between COVID-19 and various autoimmune conditions, raising intriguing questions about potential links with AOSD.
Case Presentations: Unveiling the Intersection
Illustrating the intricate interplay between COVID-19 and AOSD, the study team presented two compelling cases:
Case 1: A 29-year-old female with a known history of AOSD presented with worsening symptoms following a COVID-19 diagnosis. Despite prior disease management with corticosteroids and disease-modifying antirheumatic drugs (DMARDs), the patient experienced a flare-up characterized by fever, myalgias, and maculopapular rash. Laboratory investigations revealed leukocytosis, elevated inflammatory markers, and imaging findings suggestive of systemic involvement. Treatment involved a tailored approach with high-dose steroids and immunomodulatory therapy, highlighting the challenge of managing AOSD exacerbations in the context of COVID-19.
Case 2: A 55-year-old female without prior rheumatological history developed symptoms consistent with AOSD shortly after recovering from COVID-19. Persistent fever, polyarthralgia, and laboratory abnormalities, including leukocytosis and elevated acute-phase reactants, prompted further evaluation. Imaging studies revealed hepatosplenomegaly and lymphadenopathy, raising suspicion for systemic involvement. Treatment initiation with corticosteroids led to clinical improvement, underscoring the potential role of COVID-19 as a trigger for autoimmune dysregulation.
Discussion: Unraveling Shared Pathophysiological Mechanisms
The cases presented underscore intriguing parallels between COVID-19 and AOSD, extending beyond clinical manifestations to shared pathophysiological pathways. Both conditions exhibit systemic inflammation, characterized by elevated cytokine levels and immune dysregulation. COVID-19-induced cytokine storm shares striking similarities with the dysregulated cytokine profile observed in AOSD, implicating common inflammatory mediators such as interleukin-1 (IL-1), IL-6, and tumor necrosis factor-alpha (TNF-α).
Emerging Evidence and Clinical Implications
Mounting evidence suggests that COVID-19 may act as a trigger for autoimmune dysregulation, potentially precipitating AOSD onset or exacerbations. Observational studies have reported increased disease flare-ups in patients with preexisting autoimmune conditions during the COVID-19 pandemic, highlighting the need for heightened clinical vigilance. Furthermore, the overlapping clinical features between COVID-19 and AOSD pose diagnostic challenges, emphasizing the importance of comprehensive evaluation and tailored management strategies.
Treatment Considerations and Future Directions
In light of the observed associations between COVID-19 and AOSD, therapeutic approaches must be individualized, considering disease severity, comorbidities, and immunomodulatory agents' efficacy and safety profiles. While corticosteroids remain a cornerstone of AOSD management, emerging evidence supports the use of targeted biologic therapies, including IL-1 and IL-6 inhibitors, in refractory cases. Future research endeavors should focus on elucidating the underlying immunological mechanisms linking COVID-19 and AOSD, paving the way for novel therapeutic interventions and precision medicine approaches.
Conclusion: Navigating the Complex Interplay
The convergence of COVID-19 and AOSD underscores the intricate interplay between infectious and autoimmune processes. Shared pathophysiological pathways, clinical manifestations, and therapeutic considerations highlight the need for a multidisciplinary approach to patient care. As the medical community navigates the ongoing COVID-19 pandemic, continued research efforts are essential to unraveling the complex immunological effects of SARS-CoV-2 and its potential implications for autoimmune diseases like AOSD. By fostering collaborative research initiatives and leveraging innovative therapeutic strategies, we can strive to optimize patient outcomes and advance our understanding of the dynamic interplay between infectious triggers and autoimmune responses.
The study findings were published in the peer reviewed journal: SAGE Open Medical Case Reports.
https://journals.sagepub.com/doi/full/10.1177/2050313X241233197
For the latest
COVID-19 News, keep on logging to Thailand Medical News.