Nikhil Prasad Fact checked by:Thailand Medical News Team Jul 24, 2024 9 months, 2 days, 20 hours, 13 minutes ago
COVID-19 News: As the world grapples with the long-term consequences of COVID-19, a silent yet alarming complication has emerged. Recent research reveals a concerning link between COVID-19 and osteomyelitis of the jaw (OMJ). This
COVID-19 News report delves into the findings of a systematic review conducted by researchers from institutions across Europe, including the National and Kapodistrian University of Athens-Greece, the University of Naples “Federico II,” -Italy and the University of Groningen-Netherland, highlighting the impact of COVID-19 on the development of OMJ.
 COVID-19 can cause Osteomyelitis of the jaw
Understanding Osteomyelitis
COVID-19 can cause Osteomyelitis of the jaw
Understanding Osteomyelitis
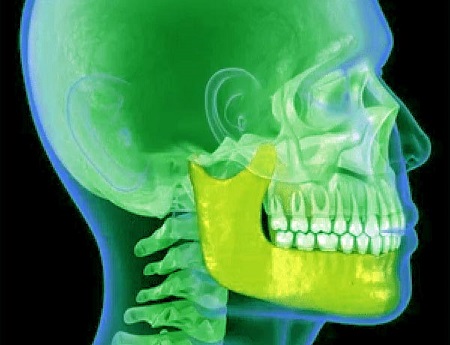
Osteomyelitis is an inflammatory condition affecting the bone and bone marrow, often leading to cell death and the formation of bone sequestrum. Traditionally caused by bacterial infections, osteomyelitis can also result from fungal or viral infections. The jaw, particularly susceptible due to its unique anatomical features, has seen a rise in osteomyelitis cases linked to COVID-19.
COVID-19's Role in Jaw Infections
The systematic review scrutinized literature from 2020 to 2024, uncovering 201 cases of jaw osteomyelitis associated with COVID-19 (COMJ). The majority of cases involved the maxilla (upper jaw) rather than the mandible (lower jaw), with a significant number presenting sinus involvement. This article explores the demographic patterns, clinical presentations, and underlying health conditions of these patients, shedding light on how COVID-19 exacerbates the risk of developing OMJ.
Key Findings
-Demographics and Health Conditions
The review highlighted a predominance of COMJ in males, accounting for 74.4% of cases, with a median age of 52.7 years. A striking finding was the high prevalence of diabetes mellitus among patients, observed in 65.1% of cases. This comorbidity, along with corticosteroid therapy used in COVID-19 treatment, significantly increased the risk of developing OMJ. Additionally, 41.5% of patients were hospitalized due to COVID-19, indicating severe infections that potentially weakened their immune systems, making them more vulnerable to secondary infections like OMJ.
-Clinical Presentations
Patients commonly presented with pain and swelling in the jaw, tooth mobility, and pus discharge. Radiological evaluations, including CT scans, played a crucial role in diagnosing the condition. The findings showed that the maxilla was predominantly affected, with 90.5% of cases involving this region. Sinus involvement was noted in nearly half of the cases, adding complexity to the diagnosis and treatment of OMJ.
-Fungal Infections: A Predominant Threat
Mucormycosis and aspergillosis emerged as the leading fungal infections associated with COVID-19 induced OMJ, identified in 51.2% and 24.9% of cases, respectively. The review underscored the role of fungal infections in exacerbating OMJ, particularly in immunocomprom
ised patients. The use of broad-spectrum antibiotics and corticosteroids during COVID-19 treatment likely disrupted normal microbial flora, creating a conducive environment for fungal overgrowth.
Treatment Approaches
Managing COVID-19 Induced OMJ poses significant challenges for healthcare providers. The review revealed a combination of surgical and non-surgical treatments employed in addressing the condition. Surgical interventions included maxillectomy (total or subtotal) and surgical debridement, while non-surgical treatments involved antifungal medications like amphotericin B and fluconazole. The extensive reliance on surgical treatments underscores the severity of OMJ and the need for aggressive management to prevent further complications.
Implications for Healthcare Providers
The findings of this review emphasize the need for heightened vigilance among dental and maxillofacial professionals. Early diagnosis and intervention are crucial in managing COMJ effectively. Healthcare providers should be aware of the potential link between COVID-19 and OMJ, especially in patients with underlying health conditions such as diabetes. This awareness can facilitate timely referrals and appropriate treatment strategies, improving patient outcomes.
Future Research Directions
While this systematic review provides valuable insights into the relationship between COVID-19 and OMJ, it also highlights gaps in current knowledge. Further research is needed to understand the mechanisms by which SARS-CoV-2 influences the development and progression of OMJ. Additionally, comparative studies focusing on different COVID-19 variants and their impact on the risk of developing OMJ could provide crucial information for tailored treatment approaches.
Conclusion
The systematic review conducted by researchers from prestigious institutions across Europe sheds light on the emerging complication of OMJ in COVID-19 patients. The findings underscore the importance of early diagnosis, aggressive management, and ongoing research to better understand and address this condition. As the world continues to navigate the long-term effects of COVID-19, healthcare providers must remain vigilant and proactive in identifying and treating complications like OMJ.
The study findings were published in the peer-reviewed journal: Journal of Clinical Medicine.
https://www.mdpi.com/2077-0383/13/15/4290
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-evidence-found-that-sars-cov-2-even-delves-into-the-skull-bones-of-those-infected
https://www.thailandmedical.news/news/dental-researchers-warn-that-covid-19-can-also-cause-osteonecrosis-of-the-jaws