Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 11, 2024 1 year, 1 month, 1 week, 1 day, 4 hours, 9 minutes ago
Medical News: Alpha-synucleinopathies refer to a group of neurodegenerative diseases marked by the accumulation of alpha-synuclein (α-syn) proteins within the brain and nervous system. Under typical circumstances, α-syn helps maintain cellular health, but when these proteins clump together, they can disrupt cell function, contributing to diseases like Parkinson's disease (PD), dementia with Lewy bodies, and multiple system atrophy. Researchers have shown that various factors, including infections and inflammation, might trigger or accelerate these conditions. Now, scientists are examining whether COVID-19 plays a role in this process.
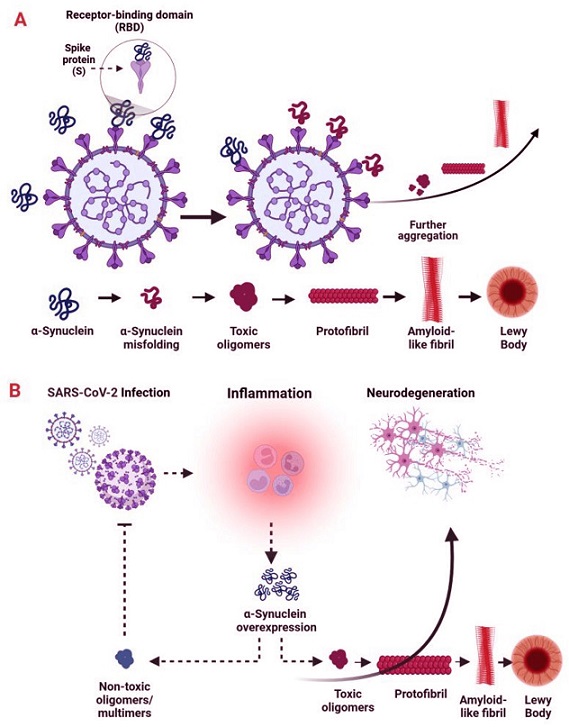
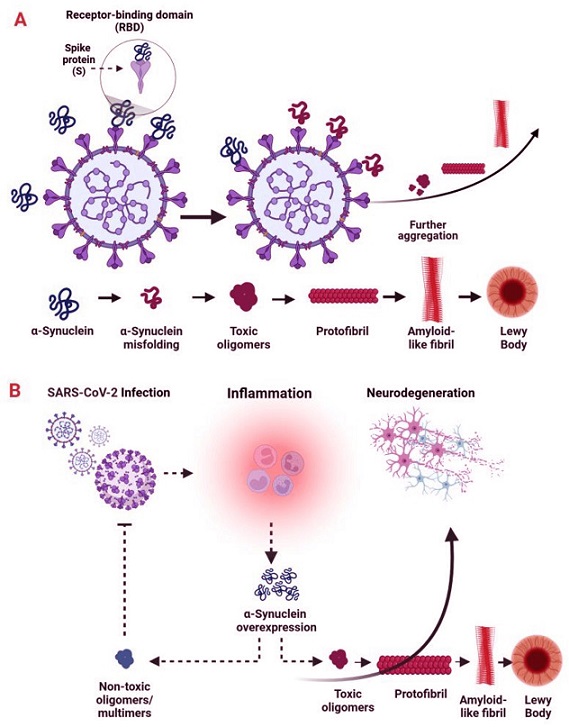 SARS-CoV-2–induced alterations in α-synuclein. (A) Potential direct interactions between the SARS-CoV-2 spike (S) protein and α-synuclein. The S protein may directly interact with α-synuclein, potentially altering its structure and increasing its propensity to misfold and aggregate. This interaction could encourage the formation of toxic α-synuclein oligomers or fibrils, which are harmful to neurons. (B) SARS-CoV-2–induced activation of α-synuclein’s immunomodulatory function. α-Synuclein plays a role in the immune system, including the modulation of inflammatory responses. When SARS-CoV-2 infects a cell, it initiates inflammatory signaling that involves microglial activation and the release of high levels of pro-inflammatory cytokines and chemokines. This inflammatory response may lead to α-synuclein accumulation and neuronal damage. Conversely, non-toxic multimers of α-synuclein could help prevent viral spread.
The Role of SARS-CoV-2 in Alpha-Synuclein Accumulation
SARS-CoV-2–induced alterations in α-synuclein. (A) Potential direct interactions between the SARS-CoV-2 spike (S) protein and α-synuclein. The S protein may directly interact with α-synuclein, potentially altering its structure and increasing its propensity to misfold and aggregate. This interaction could encourage the formation of toxic α-synuclein oligomers or fibrils, which are harmful to neurons. (B) SARS-CoV-2–induced activation of α-synuclein’s immunomodulatory function. α-Synuclein plays a role in the immune system, including the modulation of inflammatory responses. When SARS-CoV-2 infects a cell, it initiates inflammatory signaling that involves microglial activation and the release of high levels of pro-inflammatory cytokines and chemokines. This inflammatory response may lead to α-synuclein accumulation and neuronal damage. Conversely, non-toxic multimers of α-synuclein could help prevent viral spread.
The Role of SARS-CoV-2 in Alpha-Synuclein Accumulation
The SARS-CoV-2 virus, which causes COVID-19, is thought to affect brain health by promoting the aggregation of α-syn proteins. This
Medical News report examines recent research and considers whether COVID-19 could be an environmental factor that hastens or exacerbates α-syn-related disorders like PD.
One of the main concerns is that SARS-CoV-2 might directly interact with α-syn, accelerating its misfolding and aggregation. The researchers believe that these abnormal clumps of α-syn can spark inflammation, setting off a chain reaction that damages neurons. Scientists from institutions like the Polish Academy of Sciences, Cardinal Stefan Wyszyński University, and others are exploring these potential links.
Neurological Implications of COVID-19
During the COVID-19 pandemic, patients reported a range of neurological symptoms, including loss of smell, cognitive issues, and even motor disturbances similar to PD. These symptoms suggest that SARS-CoV-2 could affect α-syn function, possibly increasing the risk of long-term brain changes. Observations from autopsies have revealed that COVID-19 may even affect neurons in key brain areas, which aligns with some symptoms seen in PD.
Alpha-Synuclein in Viral Infections
In past studies, viral infections have been linked to increased levels of α-syn, possi
bly due to the body’s attempt to fight off infections. The protein plays a role in the immune response, but its accumulation could inadvertently lead to harmful clumps associated with PD. Studies have shown that viral infections can exacerbate neuroinflammatory processes, encouraging α-syn to misfold and clump together. When this happens, neurons are at risk of damage, and in severe cases, this process may lead to a lasting neurodegenerative disorder.
How SARS-CoV-2 Could Affect Brain Health
SARS-CoV-2 might be impacting brain health through several pathways. Some researchers have proposed that the virus could gain entry to the brain via the olfactory nerve, potentially explaining the loss of smell in COVID-19 patients. Once in the brain, SARS-CoV-2 could set off a cascade of neuroinflammation, prompting the immune system to release chemicals that may harm healthy neurons.
Another theory is that SARS-CoV-2 could directly interact with α-syn proteins. Laboratory studies have shown that SARS-CoV-2 proteins, like the spike protein, could bind to α-syn, increasing its tendency to misfold. This interaction may lead to toxic α-syn clusters, further damaging neurons.
Is Parkinson's Disease on the Rise?
PD is already one of the most common neurodegenerative diseases worldwide, affecting over 10 million people. Given the potential role of viral infections in PD, some researchers are concerned that COVID-19 might increase the number of PD cases or exacerbate symptoms in those already diagnosed. Long-term studies are underway to determine whether COVID-19 increases the risk of developing PD or similar neurodegenerative disorders.
Studies Linking COVID-19 and Parkinson’s Symptoms
Some studies have explored this link by examining COVID-19 patients who developed Parkinson's-like symptoms after recovering. While these symptoms often resolve, they may provide clues to the long-term effects of SARS-CoV-2 on the brain. This link between COVID-19 and PD symptoms has been noted in both human and animal studies, but more research is needed to understand its implications fully.
Future Treatment Possibilities
Researchers are exploring treatment options that could benefit both PD patients and those experiencing neurological symptoms after COVID-19. For example, anti-inflammatory medications that target specific immune pathways are being investigated. Drugs that support mitochondrial function or reduce oxidative stress are also of interest, as these could help protect neurons from the damage associated with α-syn accumulation.
Conclusion
The relationship between COVID-19 and neurodegenerative diseases like PD is complex and still under investigation. Current findings suggest that SARS-CoV-2 may contribute to neuroinflammation, α-syn misfolding, and neuronal damage, potentially leading to symptoms similar to those seen in PD. While COVID-19 does not seem to directly cause PD, it may increase the risk for certain neurodegenerative processes.
In the future, understanding this link could lead to new treatments that protect brain health and support those affected by PD. As researchers continue to uncover new details, it will be important to track how COVID-19 impacts the prevalence and progression of neurodegenerative diseases.
The study findings were published in the peer-reviewed International Journal of Molecular Sciences.
https://www.mdpi.com/1422-0067/25/22/12079
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/how-sars-cov-2-spike-protein-triggers-neurodegenerative-diseases-and-the-potential-of-metformin-as-a-therapeutic-remedy
https://www.thailandmedical.news/news/read-study-shows-sars-cov-2-n-protein-interacts-with-host-s-synuclein-proteins,-promoting-accelerated-amyloid-formation-and-parkinson-s-disease
https://www.thailandmedical.news/news/sars-cov-2-proteins-can-form-neurotoxic-amyloid-assemblies-that-are-taken-up-by-host-neurons
https://www.thailandmedical.news/news/university-of-oklahoma-study-discovers-how-the-polypeptide-sk9-from-the-envelope-protein-of-sars-cov-2-causes-parkinson-s-disease
https://www.thailandmedical.news/news/researchers-warn-that-sars-cov-2-is-triggering-neurodegenerative-diseases-like-parkinsons
https://www.thailandmedical.news/news/another-study-findings-adds-to-the-increasing-evidence-that-sars-cov-2-infection-increases-risk-of-brain-degeneration-that-will-lead-to-parkinson-s-di
(Please refer to the TMN website as there are more than 42 articles related to this topic.)