COVID-19 Causes Disruptions in Blood-Brain Barrier via Mitochondria Impairment and Endothelial Dysfunction
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 28, 2024 3 months, 3 weeks, 2 days, 4 hours, 54 minutes ago
Medical News: The COVID-19 pandemic, caused by the SARS-CoV-2 virus, has brought numerous health complications, extending far beyond the respiratory system. Among these are troubling neurological symptoms such as cognitive decline, encephalopathy, and even neurodegenerative conditions. Recent research from Parul University’s Cell and Developmental Biology Laboratory in Vadodara, India, has delved into the mechanisms behind these issues. The study provides significant insights into how COVID-19 disrupts the blood-brain barrier (BBB) by impairing mitochondria and causing endothelial dysfunction. This
Medical News report explores the findings in an accessible manner, detailing how the virus affects the brain and its protective barriers.
 COVID-19 Causes Disruptions in Blood-Brain Barrier via Mitochondria Impairment and Endothelial Dysfunction
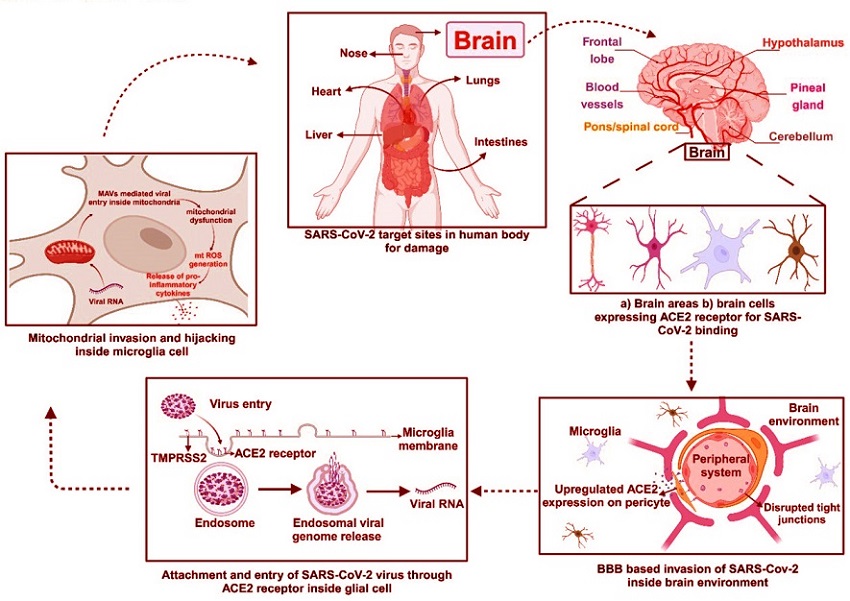
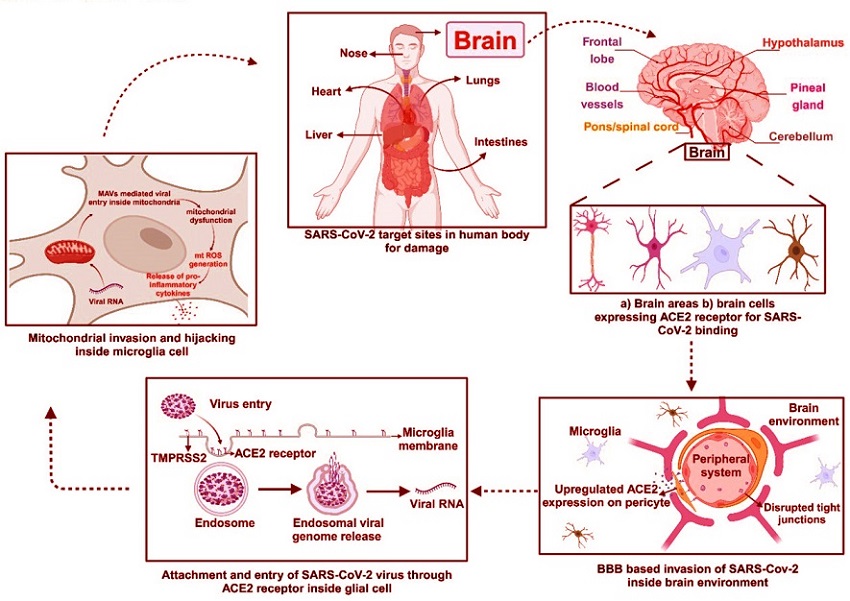
ACE2 receptor-mediated SARS-CoV-2 entry inside the human body. The expression of Angiotensin-converting enzyme 2 (ACE2) by brain region and cells facilitates the entry of viral spike protein from the peripheral system to the central nervous system. The uptake of virus genome content by the host cell results in targeted degeneration of mitochondria i.e. the powerhouse of the cell. This results in the collapse of major metabolisms of cells ultimately, causing cell death.
Understanding the Blood-Brain Barrier and Its Role
COVID-19 Causes Disruptions in Blood-Brain Barrier via Mitochondria Impairment and Endothelial Dysfunction
ACE2 receptor-mediated SARS-CoV-2 entry inside the human body. The expression of Angiotensin-converting enzyme 2 (ACE2) by brain region and cells facilitates the entry of viral spike protein from the peripheral system to the central nervous system. The uptake of virus genome content by the host cell results in targeted degeneration of mitochondria i.e. the powerhouse of the cell. This results in the collapse of major metabolisms of cells ultimately, causing cell death.
Understanding the Blood-Brain Barrier and Its Role
The blood-brain barrier is a highly selective boundary that protects the brain from harmful substances in the bloodstream. Comprised of endothelial cells, neurons, pericytes, astrocytes, and microglia, the BBB is essential for maintaining the brain’s environment and ensuring its proper function. It regulates the flow of nutrients and prevents toxic materials from entering the brain. However, the systemic inflammation caused by SARS-CoV-2 compromises this barrier, allowing harmful molecules to pass through.
This study highlights how mitochondrial dysfunction and endothelial cell activation exacerbate this breakdown. By analyzing multi-transcriptome data, the researchers uncovered specific molecular mechanisms linking COVID-19 to BBB damage, shedding light on the pathways of oxidative stress and inflammation.
The Role of Mitochondria in BBB Dysfunction
Mitochondria, often called the powerhouses of the cell, are central to cellular energy production. However, SARS-CoV-2-induced mitochondrial dysfunction triggers a cascade of adverse effects. The virus disrupts mitochondrial respiration, leading to an overproduction of reactive oxygen species (ROS). These ROS, in turn, cause oxidative stress, damaging endothelial cells and impairing their function within the BBB.
The study identified key mitochondrial genes such as MT-ND1, MT-ND2, and MT-CO1 as being significantly dysregulated in COVID-19 patients. The dysfunction of these genes results in reduced ATP production and heightened oxidative stress, contributing to the breakdown of the BBB.
r />
Endothelial Dysfunction and Inflammatory Pathways
Endothelial cells play a crucial role in maintaining the structural integrity of the BBB. The study demonstrated that SARS-CoV-2 infection leads to endothelial cell shrinkage and disintegration, disrupting tight junctions - the proteins that bind cells together to form a protective barrier. This breakdown allows inflammatory molecules and immune cells to penetrate the brain, compounding neurological damage.
The researchers observed an upregulation of genes such as GABRP and ITGB5, which regulate BBB permeability. These alterations in gene expression are directly linked to increased inflammation and oxidative stress. Moreover, pathways like oxidative phosphorylation and cGMP-PKG signaling, which are vital for endothelial health, were found to be significantly disrupted.
Systemic Inflammation and Neuroinflammation
COVID-19 is notorious for causing a cytokine storm, where an overactive immune response leads to excessive production of inflammatory molecules. This systemic inflammation exacerbates BBB dysfunction, allowing neurotoxic substances and cytokines to infiltrate the brain. The presence of SARS-CoV-2 in endothelial cells further accelerates this process, making the BBB more permeable.
One striking finding of the study is how inflammation promotes the aggregation of proteins like alpha-synuclein, a hallmark of neurodegenerative diseases such as Parkinson’s. The researchers suggest that these inflammatory processes might also increase the risk of long-term neurological complications.
Key Findings of the Study
Mitochondrial Dysfunction:
-Significant dysregulation of mitochondrial genes MT-ND1, MT-ND2, MT-CO1, and others.
-Elevated ROS levels leading to oxidative stress and endothelial damage.
Endothelial Cell Damage:
-Upregulation of ITGB5 and GABRP, compromising BBB integrity.
-Disruption of tight junction proteins and increased permeability.
Inflammation and Neurodegeneration:
-Activation of inflammatory pathways, including cytokine storms.
-Potential link to neurodegenerative conditions through protein aggregation.
Potential Therapeutic Implications
The insights from this research open avenues for targeted therapies. By focusing on mitigating mitochondrial dysfunction and endothelial damage, new treatment strategies can be developed to protect the BBB and prevent neurological complications. Biomarkers identified in the study, such as those linked to oxidative stress and inflammation, could serve as diagnostic tools for early intervention.
Furthermore, therapies aimed at reducing ROS production or enhancing mitochondrial function could alleviate BBB disruption. Anti-inflammatory treatments might also help in managing the long-term neurological effects of COVID-19.
Conclusions
The findings of this study underscore the multifaceted impact of COVID-19 on the human body, particularly its role in neurological complications. The disruption of the blood-brain barrier via mitochondrial impairment and endothelial dysfunction highlights the complex interplay between viral infections, systemic inflammation, and brain health. By elucidating these mechanisms, the researchers at Parul University have paved the way for better understanding and management of post-COVID neurological issues.
This research emphasizes the need for continued vigilance and exploration into the long-term effects of COVID-19. The identification of key pathways and biomarkers provides a solid foundation for developing targeted therapies, which could significantly improve outcomes for affected individuals.
The study findings were published in the peer-reviewed journal: Scientific Reports.
https://link.springer.com/article/10.1038/s41598-024-82180-6
For the latest COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/australian-study-finds-that-those-with-post-covid-cognitive-issues-are-likely-to-suffer-from-blood-brain-barrier-disruption-and-glutamatergic-excitoto
https://www.thailandmedical.news/news/breaking-university-of-alabama-discovers-that-mild-covid-19-causes-brain-temperature-elevation-and-free-water-increases-in-the-brain
https://www.thailandmedical.news/news/neurologists-in-a-collaborative-study-identify-stages-of-brain-damage-caused-by-covid-19-and-warns-of-future-issues-in-recovered-patients
https://www.thailandmedical.news/articles/coronavirus