COVID-19 Causes Endocrine Issues Such As Suppressed Function Of The Thyroid Gland, Suppressed Male Sex Hormone Secretion And Elevated Prolactin!
Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 19, 2023 1 year, 7 months, 1 week, 2 days, 16 hours, 44 minutes ago
COVID-19 News: The COVID-19 pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has left an indelible mark on the world. While much has been learned about the acute phase of the disease, its mid- and long-term complications, particularly those affecting the endocrine system, remain shrouded in uncertainty. In this pilot case-control study, conducted jointly by the Medical University of Bialystok in Poland, Massachusetts General Hospital in the USA, and the Broad Institute of Massachusetts Institute of Technology (MIT) and Harvard, the study team aimed to shed light on the enduring effects of COVID-19 on the endocrine system, six months after the initial infection.
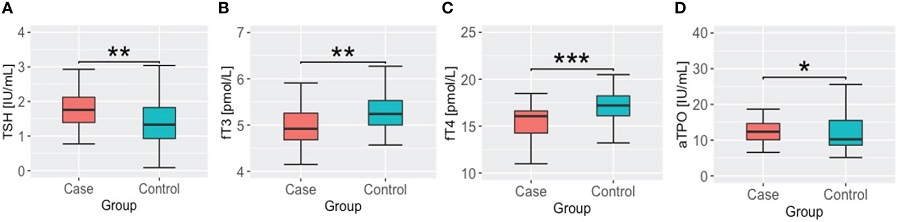
 TSH, thyroid hormone and antithyroid antibody concentrations in cases and controls groups. (A) thyroid stimulating hormone – TSH; (B) free triiodothyronine – fT3; (C) free thyroxine – fT4; (D) anti thyroid peroxidase antibody – aTPO; * - p <.05; ** - p<.01; *** - p <.001.
The Endocrine System and COVID-19
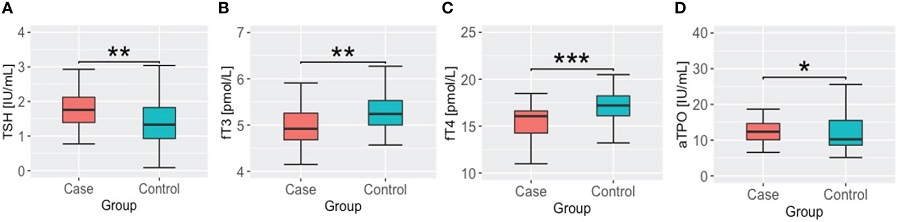
TSH, thyroid hormone and antithyroid antibody concentrations in cases and controls groups. (A) thyroid stimulating hormone – TSH; (B) free triiodothyronine – fT3; (C) free thyroxine – fT4; (D) anti thyroid peroxidase antibody – aTPO; * - p <.05; ** - p<.01; *** - p <.001.
The Endocrine System and COVID-19
Initially characterized as primarily a respiratory illness, COVID-19 has revealed itself to be a multifaceted disease with extrapulmonary manifestations, including impacts on the endocrine system. The widespread presence of the angiotensin-converting enzyme 2 (ACE2) receptor, a key cellular gateway for SARS-CoV-2, in various endocrine tissues, has rendered this system vulnerable to damage caused by the virus. ACE2 receptors, along with transmembrane serine protease 2 (TMPRSS2), are essential for viral entry into host cells, including those in the pancreas, thyroid gland, ovaries, testes, and hypothalamus. This makes the endocrine system susceptible to SARS-CoV-2 infection, raising concerns about long-term complications.
Furthermore, the pandemic has led to changes in dietary habits, often towards less healthy choices, with potential long-term consequences for endocrine health. Additionally, endocrinopathies such as obesity and diabetes have been identified as significant risk factors for severe COVID-19. The interplay between the virus and the endocrine system is complex and multifaceted, encompassing direct viral injury, endothelial dysfunction, cytokine-induced injury, and dysregulation of the renin-angiotensin-aldosterone system (RAAS). It is worth noting that the medications used to manage COVID-19, such as steroids and antiviral agents, may also have side effects on the endocrine system.
Long-COVID and Endocrine Dysfunction
Beyond the acute phase of the disease, there is mounting evidence of persistent symptoms that can last for weeks or months after the initial infection, referred to as long COVID or post-acute sequelae of SARS-CoV-2 (PASC). These lingering symptoms as covered in various past studies and
COVID-19 News reports, include fatigue, cognitive issues, depression, anxiety, joint pain, and more….and they often overlap with the clinical presentation of certain endocrinopathies, such as thyroid and adrenal gland dysfunction. Thus, understanding the impact of COVID-19 on the endocrine system is crucial, as proper
diagnosis and management of these endocrinopathies could alleviate persistent symptoms experienced by long-COVID patients.
The Role of This Study
Given the limited knowledge about the long-term effects of COVID-19 on the endocrine system, the study aimed to comprehensively assess the hormonal functions of various endocrine glands six months after the initial infection. The case-control design study involved comparing patients who had recovered from COVID-19 to age- and sex-matched subjects from a population-based study conducted before the pandemic. The study team examined multiple parameters related to metabolism and the endocrine system, including fasting glucose, insulin, lipids, body composition, thyroid function, prolactin, cortisol, testosterone, and estradiol.
Key Findings
The study yielded several significant findings:
Thyroid Function: Patients who had recovered from COVID-19 exhibited significantly lower levels of free triiodothyronine (fT3) and free thyroxine (fT4), coupled with elevated levels of thyroid stimulating hormone (TSH) and anti-thyroid peroxidase (aTPO) antibodies. These findings suggest a suppressed thyroid gland function, which could potentially lead to autoimmune hypothyroidism.
Testosterone Levels: Notably, male patients who had undergone COVID-19 showed lower levels of testosterone compared to controls. This aligns with previous research indicating that SARS-CoV-2 can directly damage Leydig cells, responsible for testosterone production. Reduced testosterone levels may have implications for male health and well-being.
Prolactin Secretion: Prolactin levels were significantly higher in COVID-19 survivors compared to the control group. Elevated prolactin is known to be a response to various stresses, including infections. Prolactin can have anti-inflammatory and immunomodulatory properties, potentially playing a role in controlling COVID-19 hyperinflammation.
Glycemic and Metabolic Parameters: In contrast to expectations, the study team did not observe significant differences in glycemic parameters, lipid profiles, liver function, body composition, cortisol levels, or estradiol levels between the COVID-19 survivor group and the control group, except for higher HOMA2-B index values, indicating increased pancreatic islet beta cell activity. This suggests that COVID-19 may not have lasting effects on these metabolic parameters.
Implications and Future Research
The findings from this pilot study provide valuable insights into the enduring impact of SARS-CoV-2 infection on the endocrine system. These insights have significant implications for clinical practice and patient management, particularly in the context of long COVID. Monitoring thyroid function after COVID-19 is essential to assess whether thyroid function returns to baseline or progresses to overt thyroid disease, enabling timely intervention. Similarly, addressing reduced testosterone levels in male COVID-19 survivors may improve their overall health and quality of life.
Despite the valuable insights gained from this study, it is important to acknowledge its limitations. These include the relatively small sample size, the case-control design, and the lack of information on the menstrual cycle phase in female participants. To gain a more comprehensive understanding of COVID-19's impact on the endocrine system, further research with larger sample sizes, more extensive hormonal assessments, including functional tests, and an observational design that captures clinical assessments before and after infection is warranted.
In conclusion, COVID-19's long-term effects on the endocrine system, as revealed in this study, encompass suppressed thyroid function, alterations in testosterone and prolactin levels, and potential autoimmune hypothyroidism. These findings underscore the importance of continued research into the interplay between COVID-19 and the endocrine system, with the goal of improving patient care and addressing the complex challenges posed by long COVID. As the number of COVID-19 survivors continues to grow, understanding and managing these endocrine-related consequences is becoming increasingly crucial in modern medicine.
The study findings were published in the peer reviewed journal: Frontiers in Endocrinology.
https://www.frontiersin.org/articles/10.3389/fendo.2023.1192174/full
For the latest
COVID-19 News, keep on logging to Thailand Medical News.