COVID-19 Causes Inflammation, Tissue Injury and Fibrosis of the Respiratory Tract and Lungs
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 26, 2024 3 months, 3 weeks, 5 days, 15 hours, 1 minute ago
Medical News: COVID-19, caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), has dramatically reshaped global health landscapes since its emergence. This highly contagious virus, originating in late 2019, primarily targets the respiratory system, leading to a cascade of complications ranging from mild symptoms to life-threatening conditions. While mild cases often resolve without severe outcomes, the virus’s potential to trigger acute respiratory distress syndrome (ARDS), inflammation, tissue injury, and fibrosis in the respiratory tract has profound implications for survivors and healthcare systems worldwide. This
Medical News report delves into these critical effects, highlighting the findings of a recent study.
 COVID-19 Causes Inflammation, Tissue Injury and Fibrosis of the Respiratory Tract and Lungs
SARS-CoV-2 and its Entry into the Respiratory System
COVID-19 Causes Inflammation, Tissue Injury and Fibrosis of the Respiratory Tract and Lungs
SARS-CoV-2 and its Entry into the Respiratory System
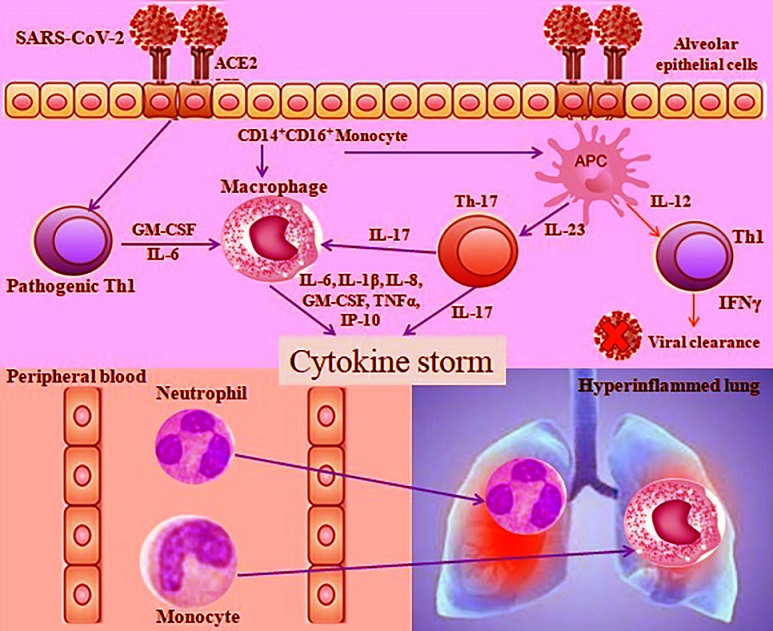
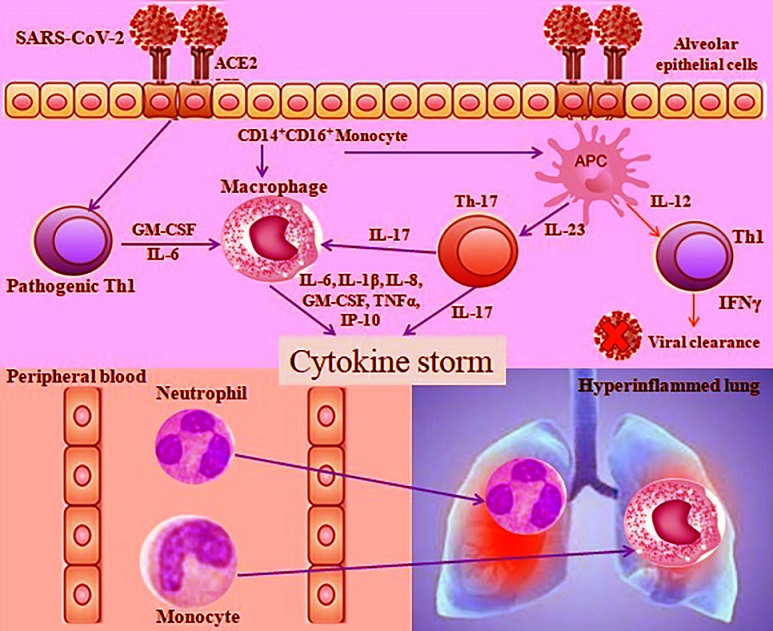
At the core of COVID-19's impact is the virus’s ability to enter and replicate within human cells, particularly in the respiratory tract. SARS-CoV-2 utilizes its spike protein to bind to the angiotensin-converting enzyme 2 (ACE2) receptors predominantly found in the epithelial cells of the nasal passages, airways, and alveoli of the lungs. This binding facilitates viral entry, replication, and subsequent cell damage. Researchers have noted that the virus’s affinity for ACE2 not only promotes its spread but also initiates inflammatory responses that can escalate into severe complications such as ARDS.
The Cytokine Storm: A Hyperinflammatory State
One of the hallmark features of severe COVID-19 is the cytokine storm - a hyperinflammatory response characterized by an overproduction of cytokines and chemokines. The immune system, in an effort to combat the virus, inadvertently harms the host by triggering widespread inflammation. This excessive response leads to tissue injury in the respiratory tract and systemic complications. Elevated levels of interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and other inflammatory markers have been strongly associated with disease severity. In critically ill patients, this storm overwhelms normal immune regulation, resulting in extensive lung damage and often necessitating intensive care interventions.
Tissue Injury and Fibrosis: Long-term Consequences
Beyond the immediate effects of inflammation, COVID-19 has been linked to structural changes in lung tissue. The persistent damage to alveolar cells disrupts the normal repair processes, paving the way for fibrosis. Pulmonary fibrosis, characterized by thickened and scarred lung tissue, impairs oxygen exchange and is a significant long-term consequence of severe COVID-19. Survivors of ARDS caused by COVID-19 are at heightened risk, as mechanical ventilation and prolonged inflammation exacerbate fibrotic changes.
The study sheds light on the mechanisms underlying this process. The researchers observed that SARS-CoV-2’s interaction with ACE2 receptors downregulates their expression, disrupting the balance of
the renin-angiotensin system. This imbalance, coupled with elevated levels of pro-fibrotic cytokines such as transforming growth factor-beta (TGF-β), drives the activation of fibroblasts and excessive deposition of extracellular matrix proteins, culminating in fibrosis.
Mechanisms of Pulmonary Damage
The damage caused by SARS-CoV-2 extends beyond the epithelial cells. Endothelial cells lining the blood vessels in the lungs are also affected, leading to increased vascular permeability and microthrombi formation. The dual assault on the alveolar and vascular compartments of the lungs amplifies the risk of severe respiratory failure.
In addition to vascular effects, SARS-CoV-2’s ability to induce mitochondrial dysfunction in host cells further contributes to its pathogenicity. The viral RNA’s interaction with mitochondrial proteins disrupts cellular energy production, triggering oxidative stress and apoptosis. These cellular processes exacerbate tissue injury and inflammation, creating a vicious cycle of damage.
The Broader Implications of COVID-19 on Respiratory Health
The repercussions of COVID-19-induced respiratory damage extend beyond acute infections. Survivors often report persistent symptoms, including breathlessness, chronic cough, and reduced lung function. Studies highlight that even patients with mild initial symptoms may experience lingering effects, raising concerns about the long-term burden of post-COVID conditions. Pulmonary fibrosis, in particular, poses significant challenges, as it is progressive and currently lacks effective treatments.
Potential Therapeutic Approaches
While no definitive cure exists for COVID-19-induced fibrosis, researchers are exploring several therapeutic strategies. Anti-inflammatory drugs, such as corticosteroids, have shown promise in mitigating the cytokine storm, albeit with potential side effects. Antifibrotic agents like pirfenidone and nintedanib, commonly used in idiopathic pulmonary fibrosis, are being evaluated for their efficacy in COVID-19-related cases. Additionally, mesenchymal stem cell therapies hold potential due to their regenerative and immunomodulatory properties.
The study also emphasizes the importance of early intervention. By targeting the inflammatory and fibrotic pathways early in the disease course, it may be possible to prevent the progression to severe complications. Future research focusing on the molecular mechanisms of SARS-CoV-2-induced fibrosis is crucial for developing targeted therapies.
Conclusions: A Call to Action
The study findings underscore the multifaceted impact of COVID-19 on the respiratory system. From inflammation to tissue injury and fibrosis, the virus’s effects are profound and far-reaching. As the pandemic evolves, understanding these mechanisms is paramount for improving patient outcomes.
Preventing and managing the long-term consequences of COVID-19 requires a multidisciplinary approach. Healthcare systems must prioritize follow-up care for survivors, ensuring timely diagnosis and treatment of conditions such as pulmonary fibrosis. Furthermore, investments in research to unravel the virus’s pathogenic pathways and develop effective therapies are imperative.
The study findings were published in the peer-reviewed International Journal of Immunopathology and Pharmacology.
https://journals.sagepub.com/doi/10.1177/03946320241310307
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-causes-vascular-fibrosis-and-vascular-remodelling
https://www.thailandmedical.news/news/67-9-percent-of-patients-who-had-severe-covid-19-pneumonia-have-evidence-of-fibrosis-three-months-after-discharge
https://www.thailandmedical.news/news/covid-19-can-lead-to-heart-fibrosis
https://www.thailandmedical.news/news/covid-19-is-not-mild-as-most-will-develop-lung-fibrosis-10-percent-of-all-lung-transplants-in-u-s-now-go-to-post-covid-patients
https://www.thailandmedical.news/news/long-term-lung-healing-even-after-mild-or-moderate-covid-19-many-could-develop-lung-fibrosis
https://www.thailandmedical.news/news/covid-19-linked-to-dangerous-lung-scarring-through-mast-cell-activation
https://www.thailandmedical.news/news/breaking-covid-19-news-44-9-percent-of-post-covid-individuals-develop-lung-fibrosis-irrespective-of-asymptomatic-or-mild-infections-jn-1-is-worse
https://www.thailandmedical.news/news/breaking-silent-tsunami-of-post-covid-lung-fibrosis-occurring-among-many-indian-researchers-warn-that-even-asymptomatics-are-at-risk
https://www.thailandmedical.news/news/university-of-virginia-study-finds-that-sars-cov-2-infections-triggers-reduction-in-circulating-monocytes-that-leads-to-persistent-post-covid-pulmonar
https://www.thailandmedical.news/news/irrespective-of-severity-40-percent-of-post-covid-pneumonia-patients-still-have-impaired-lung-diffusion-and-22-percent-developed-lung-fibrosis-a-year-
https://www.thailandmedical.news/news/great-news-most-post-covid-individuals-will-develop-lung-issues-similar-to-idiopathic-pulmonary-fibrosis-ipf-with-potential-serious-outcomes