Nikhil Prasad Fact checked by:Thailand Medical News Team Apr 26, 2024 1 year, 9 months, 1 week, 2 minutes ago
COVID-19 News: The COVID-19 pandemic, sparked by the novel coronavirus SARS-CoV-2, emerged as a global health crisis with profound repercussions on various organ systems beyond the initially recognized respiratory effects. Notably, the vascular system has come under intense scrutiny due to the diverse and often severe manifestations observed in COVID-19 patients. From endothelial dysfunction to hypercoagulable states, the virus's impact on vascular health has been extensive and multifaceted. In this
COVID-19 News, we delve into a study review by researchers from Aristotle University of Thessaloniki-Greece, Hippokration General Hospital-Greece and National and Kapodistrian University of Athens-Greece that explore the mechanisms driving these vascular alterations, explore the short-term clinical manifestations and complications, discuss the emerging concept of long-term COVID-19 and its vascular implications, and finally, outline preventive strategies and future research directions to address this critical aspect of COVID-19 pathology.
 Vascular manifestations and complications associated with SARS-CoV-2 infection
Mechanisms of Vascular Alterations in COVID-19
Vascular manifestations and complications associated with SARS-CoV-2 infection
Mechanisms of Vascular Alterations in COVID-19
The intricate mechanisms underlying vascular alterations in COVID-19 involve a cascade of events triggered by SARS-CoV-2's interaction with host cells, particularly endothelial cells (ECs). Direct viral invasion via binding to angiotensin-converting enzyme 2 (ACE2) receptors on ECs leads to endothelial injury, inflammation, and a hypercoagulable state. This endothelial damage is further exacerbated by dysregulated immune responses, mitochondrial dysfunction, and excessive inflammation, resulting in a complex interplay of factors contributing to vascular pathology.
-Endothelial Damage: SARS-CoV-2's affinity for ACE2 receptors on ECs initiates a process of endothelial injury marked by inflammation, adhesion molecule secretion, and leukocyte infiltration into arterial walls, fostering a pro-inflammatory milieu conducive to vascular dysfunction.
-Mitochondrial Dysfunction: Viral infection triggers mitochondrial reactive oxygen species (mtROS) production, leading to endothelial senescence, atherosclerosis progression, and cytokine storm induction, exacerbating vascular damage.
-Inflammation: Excessive cytokine production, known as a cytokine storm, further fuels endothelial dysfunction, thrombosis, and immune cell dysregulation, creating a vicious cycle of inflammation-driven vascular injury.
-Clot Formation: The pro-inflammatory state and endothelial glycocalyx disruption promote thrombotic events, contributing to venous and arterial thromboembolic complications commonly seen in severe COVID-19 cases.
-Immune System Dysregulation: Altered lymphocyte counts, heightened inflammatory cytokines, and immune cell activation contribute to systemic inflammation, endothelial dysfunction, and thrombotic risk, particularly in susceptible individuals with comorbi
dities.
Short-Term Vascular Manifestations and Complications
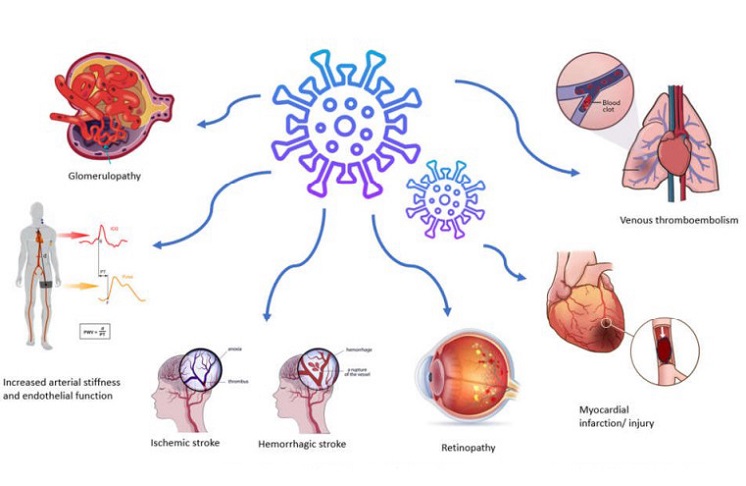
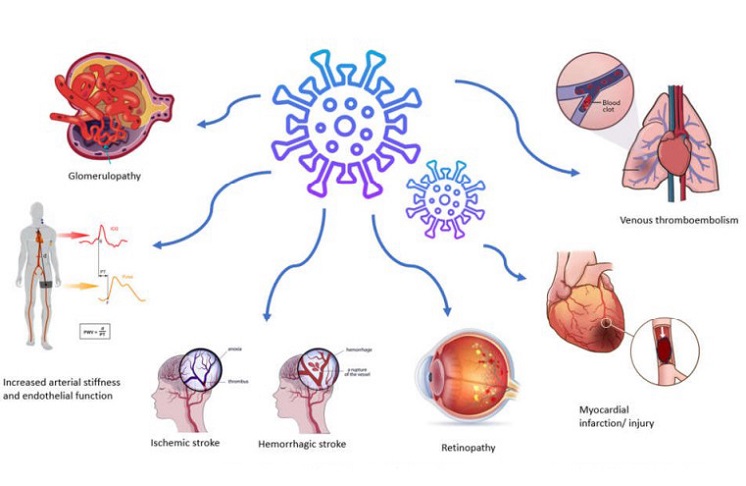
The acute phase of COVID-19 is characterized by a spectrum of vascular manifestations impacting various organ systems, including the pulmonary, cardiovascular, cerebrovascular, renal, retinal, and peripheral vascular systems.
-Thromboembolic Manifestations: Increased risk of venous and arterial thromboembolic events, such as pulmonary embolism and stroke, underscores the prothrombotic nature of COVID-19, especially in critically ill patients or those with predisposing factors.
-Pulmonary Vessels: Pulmonary involvement ranges from ARDS to pulmonary embolism, reflecting extensive endothelial dysfunction and microthrombi formation within pulmonary vasculature, contributing to respiratory compromise.
-Cardiovascular Alterations: Myocardial injury, microthrombi-related cardiomyopathy, and arrhythmias are common, emphasizing the impact of vascular dysfunction on cardiac health and prognostic outcomes in COVID-19 patients.
-Arterial Stiffness and Endothelial Dysfunction: COVID-19-induced vascular changes extend to systemic arteries, contributing to arterial stiffness, impaired endothelial function, and increased cardiovascular risk, persisting beyond the acute phase.
-Cerebrovasculature: Stroke, cerebral infarctions, and vascular inflammation highlight the cerebrovascular complications associated with COVID-19, impacting neurological outcomes and long-term vascular health.
-Nephropathy: Acute kidney injury, proteinuria, and renal microvascular changes reflect renal vascular involvement, necessitating comprehensive management strategies in COVID-19 patients with kidney complications.
-Retinopathy: Ocular manifestations, including retinal microvasculopathy and ischemic abnormalities, underscore the systemic vascular effects of COVID-19, warranting ophthalmologic evaluation in affected individuals.
Long-Term Consequences
The concept of long-term COVID-19 encompasses persistent vascular alterations and systemic sequelae beyond the acute phase, posing challenges in diagnosis, management, and understanding the enduring impact on vascular health.
-Chronic Vascular Dysfunction: Enduring endothelial dysfunction, arterial stiffness, and prothrombotic states characterize long-term COVID-19, with implications for cardiovascular morbidity, aortic aneurysm progression, and vascular calcification.
-Continued Inflammatory Response: Prolonged inflammation, mitochondrial dysfunction, and immune dysregulation sustain vascular pathology, contributing to chronic vascular complications and heightened cardiovascular risk in long COVID patients.
-Vascular Remodeling and Aneurysm Risk: Persistent alterations in arterial structure, coupled with ongoing inflammation, may accelerate vascular remodeling processes and increase the risk of aortic aneurysms, necessitating long-term surveillance and management.
-Neurovascular Complications: Long COVID's impact on cerebrovascular health extends to chronic stroke risk, neuroinflammation, and neurovascular remodeling, highlighting the need for neurological monitoring and interventions in affected individuals.
-Renal and Ocular Health: Chronic nephropathy and retinal microvascular changes underscore the systemic nature of long COVID's vascular effects, necessitating multidisciplinary care and surveillance for renal and ocular complications.
Prevention and Future Directions
Effective prevention strategies for mitigating severe vascular complications in COVID-19 involve early detection, risk stratification, antiviral therapies, vaccination, and targeted interventions addressing inflammation and endothelial dysfunction. Ongoing research aims to unravel the complexities of long COVID's vascular impact, guide clinical management, and develop innovative treatments targeting vascular pathology.
Conclusion
COVID-19's impact on vascular health transcends the acute phase, manifesting in diverse short-term complications and potentially enduring long-term consequences. Understanding the intricate mechanisms driving vascular alterations, identifying high-risk individuals, implementing preventive measures, and advancing therapeutic interventions are critical steps in addressing the vascular burden of COVID-19 and improving patient outcomes in both the acute and chronic phases of the disease.
The study findings were published in the peer reviewed journal: Life
https://www.mdpi.com/2075-1729/14/5/545
For the latest
COVID-19 News, keep on logging to Thailand Medical News.