COVID-19 Impairs Ovarian Function and Causes Premature Ovarian Failure in Women Below 40!
Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 09, 2025 2 months, 4 days, 19 hours, 17 minutes ago
Medical News: In the first few years since SARS-CoV-2 made its debut, the world was misled by ‘garbage’ researchers who claimed that the virus does not affect the reproductive system of females and that only the fertility and sexual functions of males were being affected. However new emerging studies and data are alarmingly indicating that a lot of young women are becoming infertile due to past exposure to COVID-19. A recent study conducted by researchers from the National and Kapodistrian University of Athens-Greece, the Hospital of Thun in Switzerland, Rea Maternity Hospital, IVF Athens Reproduction Center, and Athens Medical School in Greece has shed light on the concerning effects of SARS-CoV-2 infection on ovarian function. This
Medical News report highlights the significant findings, which indicate that COVID-19 may contribute to premature ovarian insufficiency (POI) in women under 40.
 COVID-19 Impairs Ovarian Function and Causes Premature Ovarian Failure in Women Below 40
What is Premature Ovarian Insufficiency (POI)?
COVID-19 Impairs Ovarian Function and Causes Premature Ovarian Failure in Women Below 40
What is Premature Ovarian Insufficiency (POI)?
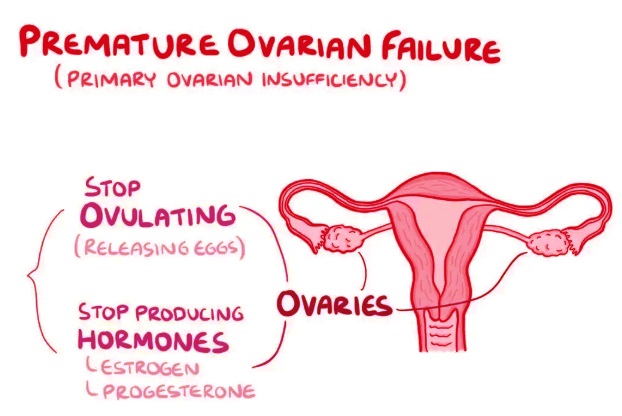
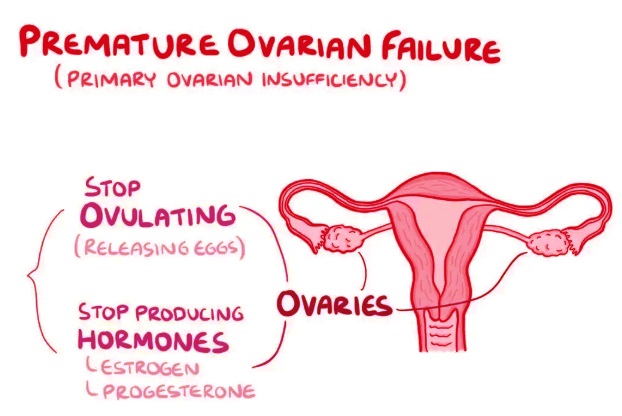
Premature ovarian insufficiency (POI), also referred to as premature ovarian failure (POF), is a condition where a woman's ovaries stop functioning normally before the age of 40. Unlike menopause, which occurs naturally around the age of 50, POI leads to early reproductive aging, causing a decline in hormone production and fertility potential. The primary symptoms of POI include irregular or missed periods, hot flashes, night sweats, vaginal dryness, reduced libido, and difficulty conceiving. Women with POI may also experience mood swings, fatigue, and an increased risk of osteoporosis and cardiovascular diseases due to lower estrogen levels.
The causes of POI can be diverse, including genetic factors, autoimmune disorders, environmental toxins, chemotherapy, radiation, and viral infections. While genetic predisposition plays a role, external factors, such as lifestyle and infections, can accelerate ovarian decline. The recent study links COVID-19 to POI, adding a new concern to the list of potential contributors to this condition.
How COVID-19 Affects Ovarian Function
SARS-CoV-2, the virus responsible for COVID-19, enters human cells via the angiotensin-converting enzyme 2 (ACE2) receptor, which is found in various tissues, including the ovaries. The study suggests that COVID-19 affects ovarian function through oxidative stress, inflammation, and immune dysregulation.
Researchers identified the following mechanisms:
-Oxidative Stress: SARS-CoV-2 increases reactive oxygen species (ROS) production, disrupting the ovarian environment. This oxidative stress can impair oocyte quality and maturation, leading to fertility issues.
-Inflammation and Immune Response: The virus triggers an overactive immune response, increasing pro-inflammatory markers like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). These inflammatory responses disrupt ovarian homeostasis and contribute to cell damage.<
br />
-Autoimmune Reactions: Some women developed anti-ovarian antibodies (AOAs) after COVID-19 infection. AOAs attack ovarian tissues, further leading to ovarian insufficiency and reduced reproductive potential.
Key Findings from the Study
The researchers analyzed hormonal levels, oocyte quality, and ovarian reserve in women who had recovered from COVID-19. Their findings revealed:
-Decreased Anti-Müllerian Hormone (AMH) Levels: AMH is a key marker of ovarian reserve. Many women post-COVID-19 exhibited lower AMH levels, indicating reduced ovarian function.
-Elevated Follicle-Stimulating Hormone (FSH) Levels: Higher FSH levels were observed in a significant proportion of women, suggesting that the ovaries were not responding adequately to hormonal signals.
-Impaired Oocyte Maturation: The study found that COVID-19-exposed women had fewer high-quality mature eggs (metaphase II oocytes) compared to non-infected women.
-Changes in Follicular Fluid Composition: Follicular fluid, which surrounds developing eggs, showed altered lipid profiles and the presence of anti-SARS-CoV-2 antibodies. These changes may contribute to decreased oocyte viability and fertilization potential.
The Broader Impact on Female Fertility and Reproductive Health
The study findings raise concerns about COVID-19's impact on female fertility. While some of the hormonal disruptions may be temporary, the long-term implications remain unclear. Women recovering from COVID-19 who plan to conceive may require additional fertility assessments. The findings also suggest that COVID-19 could accelerate ovarian aging in some cases, leading to early menopause and increased risks of osteoporosis and cardiovascular diseases.
Furthermore, the presence of ACE2 receptors in the uterus, fallopian tubes, and placenta indicates that the virus may impact not only ovarian function but also implantation and pregnancy outcomes. Studies have also raised concerns about increased risks of miscarriage, stillbirth, and pregnancy complications among women who contracted COVID-19 during their reproductive years. These aspects highlight the need for continuous research into how the virus affects female reproductive health beyond just ovarian function.
Clinical Implications and Recommendations
Given the potential impact of COVID-19 on ovarian function, healthcare providers should consider the following recommendations:
-Routine Hormonal Monitoring: Women who have recovered from COVID-19, especially those experiencing irregular menstrual cycles or fertility issues, should undergo regular testing for AMH, FSH, and estradiol levels.
-Early Fertility Assessments: Women planning pregnancy or undergoing assisted reproductive technology (ART) should be aware of potential ovarian reserve changes post-COVID-19. Doctors may recommend ovarian reserve testing and personalized fertility treatments.
-Anti-Inflammatory and Antioxidant Support: Supplements such as CoQ10, vitamin C, and vitamin E may help reduce oxidative stress and support ovarian health.
-Long-Term Follow-Up: Continuous monitoring is necessary to determine whether COVID-19-related ovarian dysfunction has lasting effects.
Future Research and Unanswered Questions
While the study provides valuable insights, many questions remain unanswered. Researchers stress the need for long-term studies to assess whether the observed hormonal disruptions are reversible or permanent. Future research should also investigate how multiple COVID-19 infections might impact ovarian function over time. Additionally, more data is needed to determine if the severity of the infection correlates with the degree of ovarian dysfunction.
Conclusion
The emerging evidence from this study suggests that COVID-19 can impair ovarian function and increase the risk of premature ovarian insufficiency in women under 40. The virus disrupts key reproductive processes through oxidative stress, inflammation, and immune dysregulation. While some effects may be temporary, the potential for long-term reproductive consequences cannot be overlooked. Healthcare providers should prioritize ovarian health monitoring in women recovering from COVID-19 to mitigate possible fertility issues.
The study findings were published in the peer-reviewed journal: Biomedicines.
https://www.mdpi.com/2227-9059/13/2/407
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/breast-cancer-rates-rising-among-younger-women
https://www.thailandmedical.news/news/covid-19-news-yet-another-case-report-showing-that-sars-cov-2-infections-can-cause-genital-ulcers-in-women
https://www.thailandmedical.news/news/breaking-covid-19-news-medical-researchers-from-portugal-warn-that-sars-cov-2-infections-can-lead-to-vulvar-ulceration-in-girls-and-women
https://www.thailandmedical.news/news/breaking-sars-cov-2-causes-aggressive-breast-cancer-progression-and-manipulates-tissue-stem-cells-in-the-tumor-microenvironment