Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 13, 2025 1 month, 6 hours, 9 minutes ago
Medical News: Alarming Discovery in Long COVID Patients
A groundbreaking new study conducted by researchers from The University of Texas at Austin Dell Medical School and The University of Michigan Medical School-USA has revealed that many Long COVID sufferers are experiencing neuropathy due to the presence of anti-ganglioside autoantibodies. The study, which analyzed nearly a thousand patients, provides compelling evidence that the SARS-CoV-2 virus may trigger an autoimmune response leading to nerve damage.
Long COVID, also known as Post-Acute Sequelae of SARS-CoV-2 Infection (PASC), is a debilitating condition affecting millions worldwide. While symptoms vary, neuropathy - damage or dysfunction of nerves - is among the most common and persistent issues reported by patients. This
Medical News report highlights critical findings that shed light on how SARS-CoV-2 affects the nervous system and offers hope for potential treatment options.
 COVID-19 Induced Anti-Ganglioside Autoantibodies is Causing Neuropathy in Many
Study Details and Key Findings
COVID-19 Induced Anti-Ganglioside Autoantibodies is Causing Neuropathy in Many
Study Details and Key Findings
The research team conducted an extensive analysis of 977 adults diagnosed with Long COVID at Dell Medical School. Participants underwent comprehensive clinical assessments, including skin punch biopsies, metabolic and immune profiling, and laboratory testing for autoantibodies. The goal was to determine the underlying causes of neuropathy and assess whether autoimmunity played a significant role.
High Prevalence of Neuropathy
The study found that 55% (534 out of 977) of Long COVID patients reported symptoms of neuropathy. These symptoms included numbness, tingling, burning pain, and abnormal sensitivity to touch, often severely impacting daily life. To objectively measure nerve damage, 85 patients underwent skin punch biopsies.
The results were alarming:
-56.5% of those tested showed small fiber neuropathy
-38.8% had reduced epidermal nerve density
-29.3% exhibited a loss of sweat gland nerve fibers
These findings confirm that Long COVID is linked to significant damage to both sensory and autonomic nerves.
The Role of Autoimmunity
One of the most striking discoveries was the presence of anti-ganglioside autoantibodies (AGAs) in 25% of patients with Long COVID neuropathy.
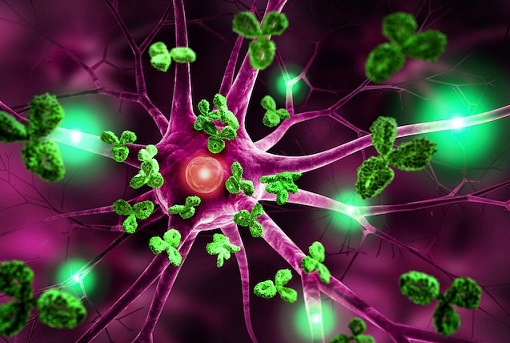
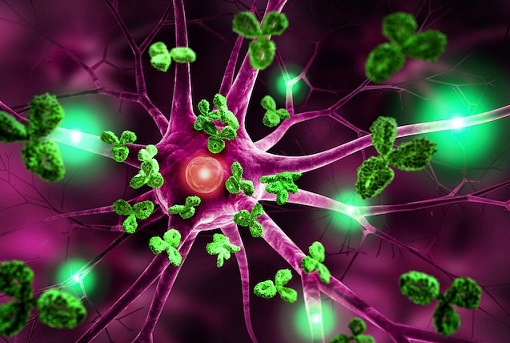
Gangliosides are vital molecules found in nerve cell membranes, and antibodies targeting them can lead to nerve dysfunction, similar to what is seen in Guillain-Barré Syndrome (GBS), an autoimmune condition that can cause paralysis.
The researchers detected various types of AGAs, including GM1, Asialo-GM1, GM2, GD1a, GD1b, and GQ1b. Notably, Asialo-GM1 was the most prevalent in patients with confirmed small fiber neuropathy, indicating a potential link between specific autoantibodies and the type of nerve damage.
&a
mp;nbsp;
Persistence of Autoantibodies Over Time
The team performed longitudinal testing on a subset of patients with AGA positivity and found that these autoantibodies persisted for more than a year in some individuals.
This prolonged presence of AGAs may explain why neuropathic symptoms in Long COVID patients do not resolve over time and suggests that SARS-CoV-2 may be triggering a sustained autoimmune response.
Can Neuropathy Be Treated?
Intravenous Immunoglobulin (IVIG) Therapy Shows Promise
As part of the study, eight patients with Long COVID neuropathy underwent intravenous immunoglobulin (IVIG) therapy, a treatment commonly used for autoimmune disorders. Encouragingly, all patients reported an improvement in their neuropathic symptoms after receiving IVIG:
-37.5% (3 out of 8) reported significant improvement
-62.5% (5 out of 8) reported moderate symptom relief
Interestingly, even in patients with persistent AGAs, IVIG seemed to alleviate symptoms, suggesting it may help by modulating the immune response rather than directly eliminating autoantibodies.
Implications and Future Research
The findings from this study suggest that Long COVID-associated neuropathy is, in many cases, an autoimmune-driven condition rather than being solely caused by metabolic or toxic factors. The presence of AGAs in a significant portion of patients supports the theory that SARS-CoV-2 can trigger an immune system attack on nerve cells.
Moreover, the response to IVIG therapy provides a potential pathway for treatment, offering hope for thousands suffering from nerve damage due to Long COVID. However, larger clinical trials are needed to confirm these results and optimize treatment protocols.
Conclusion
This research represents a major step forward in understanding the neurological complications of Long COVID. The detection of anti-ganglioside autoantibodies in one out of four neuropathy patients strongly suggests that an autoimmune response is at play. The persistence of these antibodies and their association with nerve damage further supports this hypothesis.
With no universally effective treatment for Long COVID neuropathy currently available, the promising results from IVIG therapy warrant further investigation. If confirmed through larger studies, immunotherapy could become a key tool in managing Long COVID-related nerve damage, improving the quality of life for many sufferers.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.medrxiv.org/content/10.1101/2025.03.04.25323101v2
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/scientists-discover-a-highly-conserved-region-in-the-sars-cov-2-spike-protein-that-triggers-harmful-autoantibodies
https://www.thailandmedical.news/news/it-was-wrong-to-have-used-the-spike-proteins-in-the-covid-19-vaccines-as-they-can-elicit-many-kinds-of-pathogenic-autoantibodies
https://www.thailandmedical.news/news/list-of-86-of-167-autoantibodies-that-covid-19-infections-and-vaccines-induces-in-the-human-host-part1
https://www.thailandmedical.news/pages/thailand_doctors_listings
https://www.thailandmedical.news/articles/hospital-news