COVID-19 Induces Epigenetic Changes in Nasal Cells, Resulting in Long-Term Breathing Issues
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 24, 2025 3 weeks, 1 day, 15 hours, 57 minutes ago
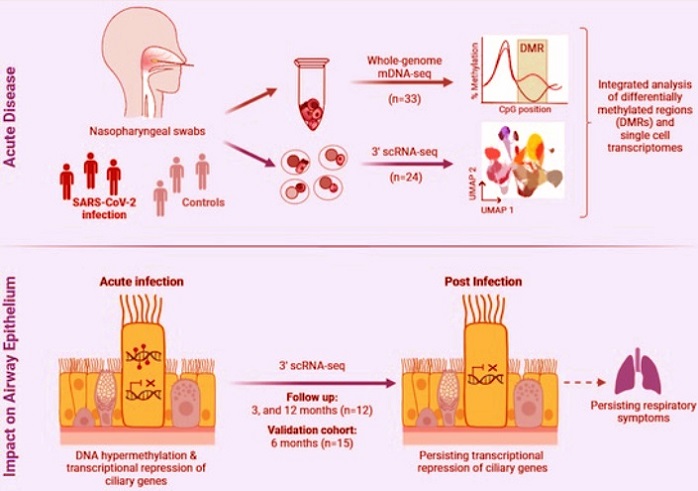
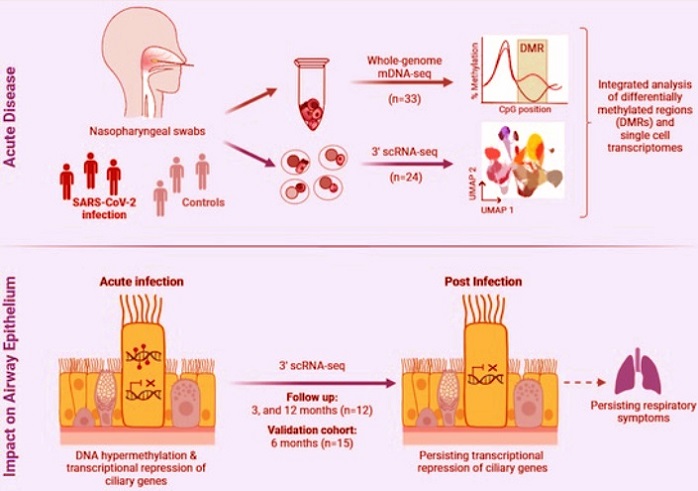
Medical News: In a groundbreaking new study, German researchers have uncovered how a SARS-CoV-2 infection may leave behind silent, long-lasting scars in the body’s respiratory system - even long after the virus is gone. The study reveals that DNA methylation changes, a form of epigenetic modification, occurring during the acute phase of COVID-19, can have prolonged effects on gene activity in nasal epithelial cells, particularly the ciliated cells responsible for clearing mucus and pathogens from the airways.
 COVID-19 Induces Epigenetic Changes in Nasal Cells, Resulting in Long-Term Breathing Issues
COVID-19 Induces Epigenetic Changes in Nasal Cells, Resulting in Long-Term Breathing Issues
The international research team was led by scientists from the Berlin Institute of Health at Charité - Universitätsmedizin Berlin, Freie Universität Berlin, University Hospital Leipzig, Heidelberg University Hospital, the Max Planck Institute for Molecular Genetics, the German Center for Lung Research, and other associated institutions. This
Medical News report explores how these changes could explain persistent respiratory symptoms in many people experiencing post-COVID-19 conditions - especially those struggling with breathlessness and chronic fatigue.
COVID-19 Leaves More Than Just a Temporary Mark
Most people associate COVID-19 with symptoms that resolve within a few weeks. But for millions worldwide, the infection has triggered long-term complications now recognized as part of post-COVID-19 condition (PCC), or “long COVID.” One of the most common and debilitating symptoms is difficulty breathing or unexplained shortness of breath that persists for months.
What makes these symptoms so hard to treat is that in many cases, imaging and routine lung function tests come back normal. Scientists have been left wondering - what is going on beneath the surface?
To find answers, the researchers turned to the body’s first line of defense against airborne viruses - the nasal epithelial cells. These cells, especially ciliated cells that sweep out dust, mucus, and pathogens, play a vital role in respiratory health. Using advanced genomic tools, the team looked at how COVID-19 alters DNA methylation, a chemical process that regulates gene expression without changing the DNA code itself.
Long Term Silencing of Key Genes in the Airway
The study involved 33 individuals - 19 COVID-19 patients and 14 healthy controls. Samples were collected from the nasal cavity during the acute phase of infection and, in some cases, followed up at 3-, 6-, and 12-months post-infection. The team employed whole-genome DNA methylation sequencing (mDNA-seq) and single-cell RNA sequencing (scRNA-seq) to examine how gene expression and DNA methylation patterns changed over time.
They discovered 3,112 regions in the genome that were differentially methylated in COVID-19 patients compared to healthy individuals. Interestingly, over 80 percent of these changes were "hypermethylations" - where certain parts of the DNA gained extra methyl groups, effectively s
witching off the genes in those regions.
In particular, genes involved in the development and function of cilia were heavily affected. These included RSPH9, DNAH3, DNAH5, IFT122, IFT46, RFX3, and others - genes critical to cilia formation and motility. The research showed that these genes were not only turned off during the acute phase of COVID-19 but stayed suppressed even 12 months later in some patients, especially those who reported ongoing respiratory issues.
Loss of Ciliary Function May Be Root of Long COVID Breathing Issues
The long-term suppression of ciliary genes was especially troubling. Cilia are tiny, hair-like structures on the surface of nasal and airway cells that beat rhythmically to push mucus and trapped particles out of the airways. When these are impaired, the respiratory system becomes more vulnerable to infections, inflammation, and inefficient clearing of airways - leading to chronic symptoms like breathlessness and coughing.
Even a year after infection, the gene activity associated with ciliogenesis (the creation of new cilia) had not fully recovered in many patients. While basal and secretory epithelial cells showed signs of recovery, the ciliated cells remained transcriptionally repressed. This persistent gene suppression could prevent new, healthy cilia from forming properly, even in cells that have regenerated.
Furthermore, the study revealed that patients who continued to experience respiratory symptoms six months after infection had significantly lower expression levels of these crucial cilia-related genes compared to asymptomatic individuals. This suggests that the severity of long-term symptoms could be directly tied to these molecular changes.
The Immune System's Role and Epigenetic Reprogramming
Interestingly, not all methylation changes led to gene repression. Some areas of the genome underwent hypomethylation - where methyl groups were removed - leading to increased gene activity. These regions were mostly associated with immune-related genes like CCR1, CCR2, and CCR5, particularly in macrophages.
This suggests that while the immune system remained hyperactive, the epithelial cells responsible for normal respiratory function became weakened.
The researchers emphasized that these changes are not genetic mutations, but epigenetic reprogramming - meaning the environment or viral infection itself can change how genes behave, potentially in a long-lasting manner. These epigenetic changes can persist through many cell divisions, effectively imprinting a memory of the infection in respiratory tissues.
This may explain why some patients continue to suffer long after the virus has been cleared from the body. The airway cells may have been reprogrammed during the infection to express certain genes less - or not at all - and this altered state could contribute to lingering symptoms.
Independent Validation Supports Link to Long COVID
To further support their findings, the researchers examined an independent cohort of 15 people who had mild COVID-19 and were never hospitalized. Samples taken six months post-infection again revealed reduced activity in ciliary genes in patients who reported persistent breathing problems compared to those who had recovered fully.
Key genes like RFX3, DNAH3, and EZR were consistently found to be repressed in individuals with post-COVID-19 respiratory symptoms. This strengthens the argument that the virus leaves behind molecular changes that can directly interfere with respiratory function.
Conclusions and Future Implications
This study provides one of the first detailed looks into how COVID-19 can create long-lasting epigenetic alterations in the body’s respiratory lining. Unlike previous studies that focused on blood samples, this research directly examined nasal epithelial cells - the initial site of SARS-CoV-2 infection.
By showing that DNA methylation changes can persist for months and are linked to transcriptional silencing of vital ciliary genes, the study uncovers a potential mechanism for long-term symptoms like breathlessness, even in patients who had mild illness. It raises the possibility that each reinfection with SARS-CoV-2 might increase the risk of accumulating further damage through these subtle but lasting molecular scars.
For the millions affected by post-COVID-19 condition, these findings highlight the importance of continued research and monitoring - even for those with seemingly minor initial infections. Understanding how the virus rewires our gene expression may help researchers develop therapies to reverse these changes or prevent them altogether.
The study also calls for the development of diagnostic tools to detect epigenetic signatures of past COVID-19 infections, which could help identify individuals at risk for long-term symptoms.
The study findings were published in the peer reviewed journal: EMBO Molecular Medicine.
https://www.embopress.org/doi/full/10.1038/s44321-025-00215-5
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/u-s-nih-study-shows-that-omicron-spike-proteins-confers-enhanced-infectivity-and-interferon-resistance-to-sars-cov-2-in-human-nasal-tissue
https://www.thailandmedical.news/news/understanding-how-covid-19-alters-airway-stem-cells-and-the-potential-of-stem-cell-therapy
https://www.thailandmedical.news/news/covid-19-news-u-s-study-using-human-intranasal-micro-optical-coherence-tomography-imaging-validates-that-covid-19-causes-ciliary-dysfunction
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/pages/thailand_doctors_listings